When patients come to the ED and are diagnosed with pneumonia, it can be confusing to figure out which antibiotics to administer. Previous thinking separated community acquired pneumonia (CAP), hospital acquired pneumonia (HAP), and health-care associated pneumonia (HCAP). However, health-care associated pneumonia has been dropped from the newest treatment guidelines published in 2016 because studies found that many patients initially thought to be at higher risk for multi-drug resistant infections falling under HCAP criteria would have been appropriately treated with empiric CAP antibiotic therapy.
CAP
Traditionally azithromycin alone was used to treat CAP however since 2016 this has been recommended against because of changing resistance patterns. Given that HCAP has been removed from the guidelines, we now consider all PNA contracted in the outpatient setting CAP and to determine treatment we screen for MRSA and pseudomonas risk factors (HAP is PNA contracted 48 hours after admission). This makes treatment more complex because not every patient gets the same inpatient or outpatient treatment.
The chart below from UpToDate summarizes risk factors for MRSA and Pseudomonas.

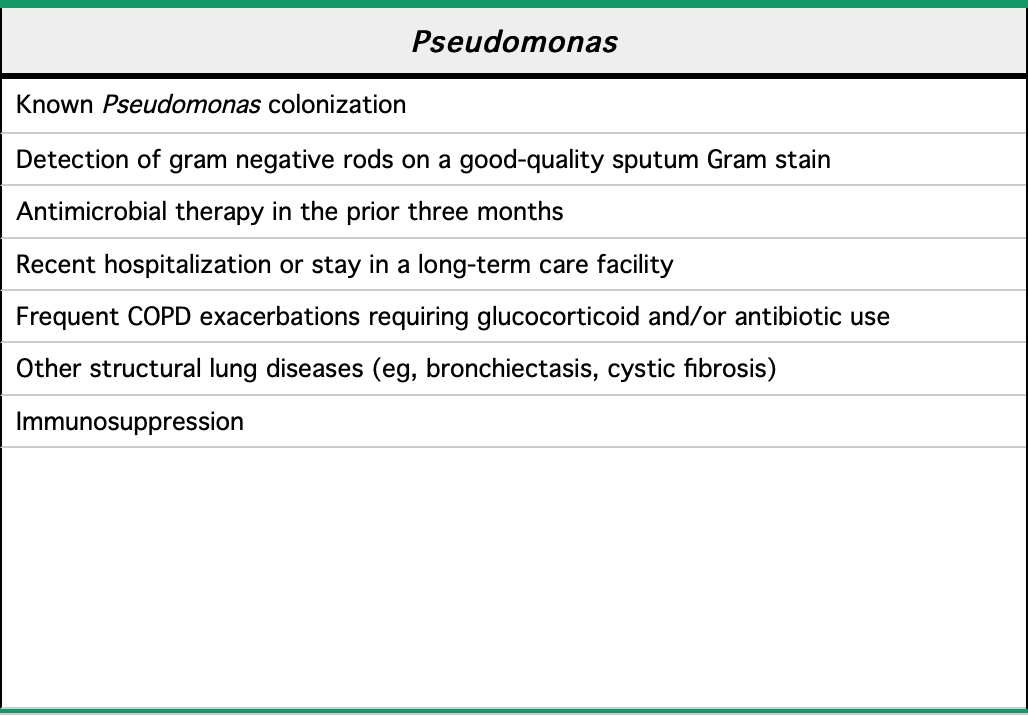
If the patient has risk factors for MRSA or pseudomonas, antibiotics that cover those specifically should be included in the patient’s regimen. Previously when HCAP was in the guidelines, vancomycin and a pseudomonas covering antibiotic such as zosyn or cefepime were used on all HCAP patients. Now that we screen for risk factors, vancomycin plus a narrow spectrum beta lactam or cephalosporin can be used for patients with MRSA risk; for patients with pseudomonas risk without MRSA risk an extended spectrum beta lactam antibiotic or cephalosporin can be used without vancomycin. This allows narrower coverage and helps prevent the development of further resistance.
The most common recommend regimen for outpatient therapy includes a beta lactam and azithromycin to help cover strep appropriately given resistance as well as to cover for atypical organisms. Possible dosing would be:
- Augmentin XR 2g BID or Amoxicillin 1g TID + Azithromycin 500mg on day 1 followed by four days of 250mg once daily. Total course 5 days total for both antibiotics.
The biggest difference of this from prior recommendations is that we now are using two antibiotics for low risk outpatient CAP because of evolving resistance to azithromycin.
In some medical systems doxycycline alone could be used to treat CAP given that it covers both strep and atypical organisms, however in our regional area strep is too resistant to doxycycline to recommend this. Another option includes single antibiotic treatment with levofloxacin however it is also not routinely recommended as there is concern its use will increase fluoroquinolone resistance of respiratory pathogens (and levofloxacin is one of our few options to cover pseudomonas with an oral antibiotic). If the patient has pseudomonas risk factors, levofloxacin should be used to appropriately cover the patient for strep, the atypicals, and pseudomonas. If the patient has MRSA risk factors, usually a combination such as a beta lactic plus doxycycline is used to help appropriately cover strep, the atypicals, and MRSA.
Inpatient CAP
If you have decided to admit the patient, you can use the DRIP (Drug Resistance in Pneumonia) score to determine if they are at risk for community acquired drug-resistant pneumonia. This was developed to reduce the use of broad spectrum antibiotics on patients who do not require them.
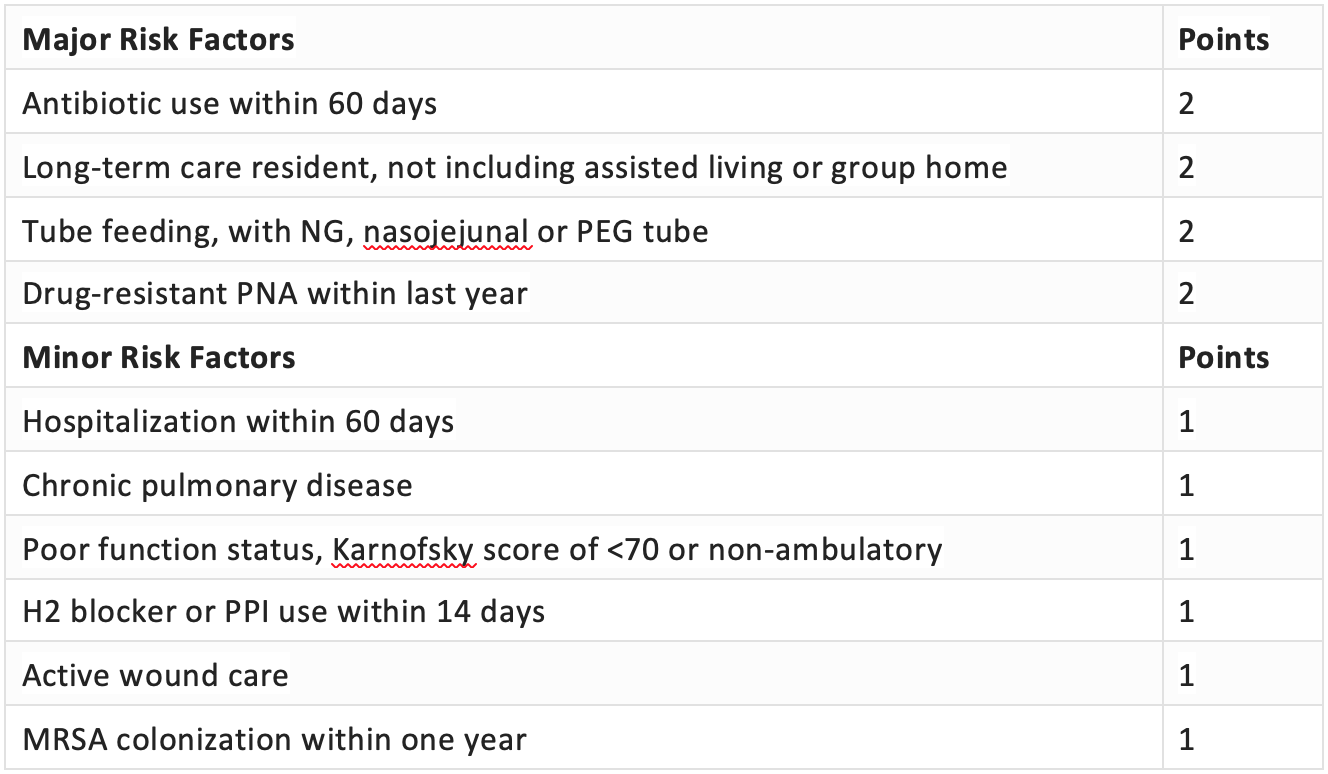
Interpretation:
DRIP score <4, patients do not need broad-spectrum antibiotics.
DRIP score ≥4, broad spectrum antibiotics likely necessary.
DRIP score <4:
Inpatient regimens include:
- Ceftriaxone 1g IV daily + Azithromycin 500mg IV daily
- Ampicillin/ Sulbactam 1.5g IV Q6H + Azithromycin 500mg IV daily
If the patient has MRSA risk factors, is post-influenza, or has radiographic evidence of cavitary lesions/necrotizing pneumonia, add Vancomycin IV.
Drip score ≥4
Broader spectrum antibiotics should be administered to cover for pseudomonas and/or MRSA. Example regimens include:
- Piperacillin/Tazobactam 3.375g Q8H IV
- Cefepime 1g IV daily
If risk factors for MRSA are present, add Vancomycin IV.
Summary:
- HCAP has been removed from the guidelines. We now differentiate PNA by CAP or HAP
- When treating CAP, determine if the patient has risk factors for pseudomonas or MRSA when choosing antibiotics
- Azithromycin alone is no longer recommended for the treatment of CAP
- Not all admitted patients with PNA need broad spectrum coverage
- The drip score can help narrow antibiotics for inpatient PNA treatment


Nice summary. Great work pullling in the DRIP score.
LikeLike