42 year old female presents to Emergency Department with a chief complaint of vision changes.
Patient states that has has been having vision changes in her right eye starting two weeks prior. She denies injury to the eye and recent infections and does not use contact lenses. Patient also states it first started out as pain in her right eye with mild blurriness that progressed gradually. At the time of presentation in the ED, she was unable to see out of the medial part of her right eye.
The patient does have a PMH of migraines and meningioma
On exam there was decreased visual acuity in the right eye. She was able to see movement to the lateral aspect, however no movement visualized to medial aspect.
Ocular ultrasound was ordered and found a retinal detachment with concern for macular off detachment. The patient was then referred to an ophthalmologist for definitive care.
Retinal Detachment
When the retina becomes detached it allows fluid to get behind the retina. Retinal detachments are often painless. A patient can also have floaters (tiny specks that appear in one’s vision), flashes of light, blurred vision, gradual loss of peripheral vision, and a curtain-like veil in vision.
There are a number of ways that retinal detachment can occur but the most common are trauma, family history of tears, myopia, cataracts surgery, and increase in intraocular pressure.
Diagnosis starts off with getting a clear and accurate history of the patient and from there you will need a suspicion for retinal detachment. The tests that have shown to have very good sensitivity and specificity are the fundoscopy and ultrasound.
Patients with retinal detachments should be referred to ophthalmology for definitive treatment.
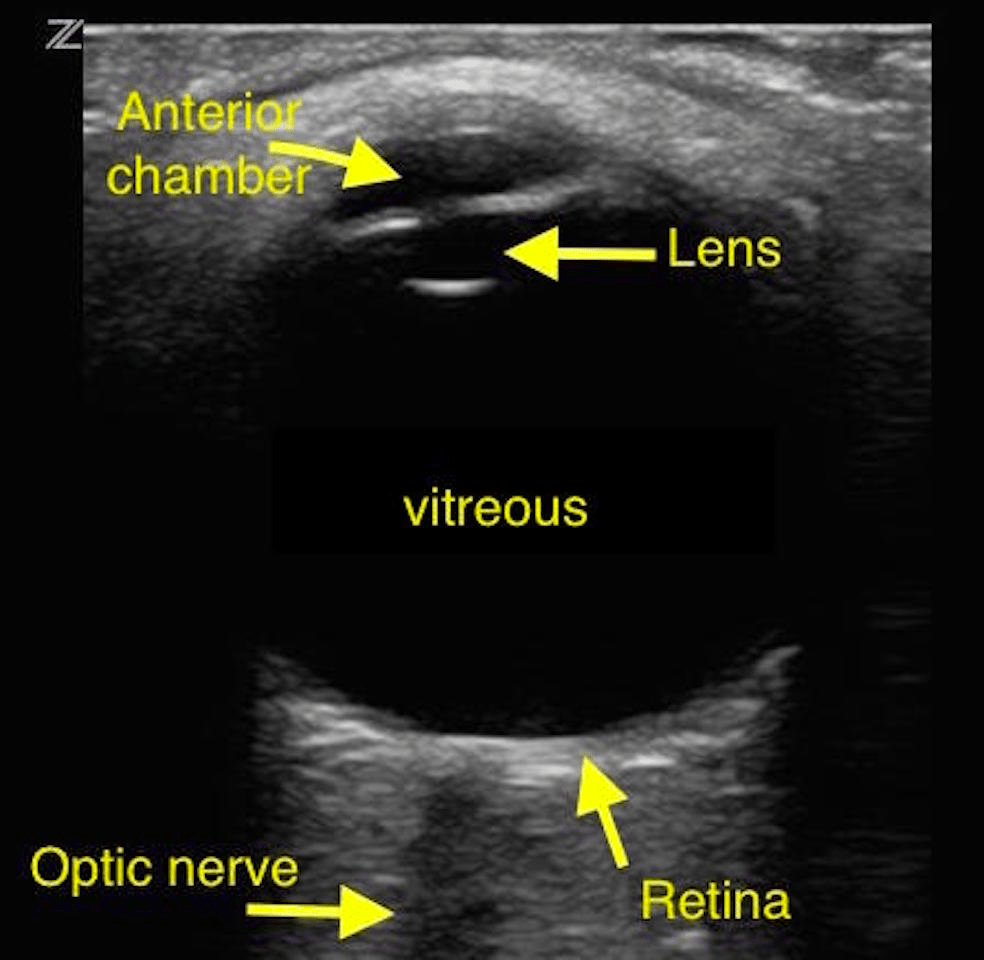
Ultrasound is device that uses sound waves to create an image of an area of interest. When using an ocular ultrasound we use the linear probe due to its high frequency and the proximity of the area in question. This gives a great image to go by.
The picture below shows normal anatomy of the eye which can be seen with an ultrasound.
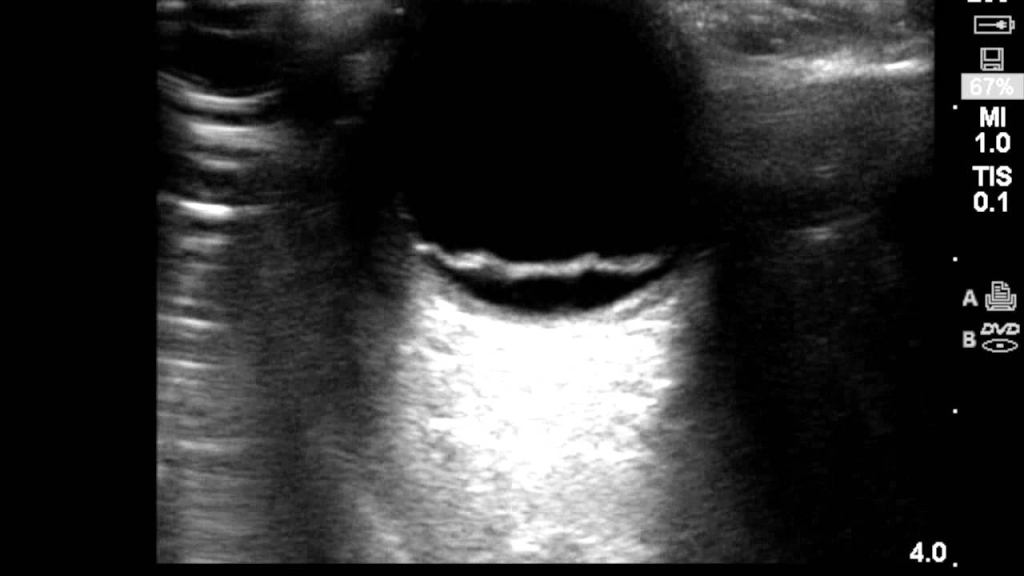
The following represents a retinal detachment which looks like the retina is floating in the vitreous instead of connected to the flat surface in the normal eye.
Attending Note
When performing an ocular ultrasound you want to use the linear probe and obtain views in both transverse and sagittal planes. It is good to get a video sweeping through the area with special care to not perform this exam on a suspected globe rupture. Using liberal amounts of ultrasound gel allows for less pressure to the globe, while tegaderm may be used to protect eye from ultrasound gel.
Retinal detachments will anchor at the posterior eye near the optic nerve, unlike most posterior vitreous detachments. The macula lies lateral to the optic nerve. When the retinal detachment goes all the way to the lateral portion of the optic nerve, suspect macular-off retinal detachment. When the retinal detachment does not reach the lateral portion of the optic nerve, suspect macular-on retinal detachment, which requires more emergent surgery to save eyesight.
An excellent guide to this ultrasound and in depth techniques may be found here
In our case we found a macular-off retinal detachment, as seen in the pictures above.
Written by: Branden Riggins, DO
Peer reviewed and edited by: Rossi Brown, DO
References
- http://www.aliem.com/ocular-ultrasound-retinal-detachment-posterior-vitreous-detachment/
- Jorge G Arroyo, MD, MPH (2020) Retinal Detachment. Jane Given MD (ED). Retrieved Jan. 14, 2021. From: https://www.uptodate.com/contents/retinal-detachment
- Lee Johnson, MS III. Ocular ultrasound. Core EM, 29 April 2019, https://coreem.net/core/ocular-ultrasound/


You must be logged in to post a comment.