Troubleshooting the Ventilator
Terms to know:
- Tidal Volume (TV)= amount of air that moves in or out of the lungs with each respiratory cycle
- Plateau Pressures (PPlat)= reflect pulmonary compliance as well as the pressure applied to small airways and alveoli. It can be measured by applying a brief inspiratory pause after ventilation.
- Peak Pressures (PIP)= This is the summation of pressure generated by the ventilator to overcome airway (ETT and bronchus) resistance and alveolar resistance to attain peak inspiratory flow and to deliver desired tidal volume.
- Barotrauma= Pulmonary barotrauma from invasive mechanical ventilation refers to alveolar rupture due to elevated transalveolar pressure, air leaks into extra-alveolar tissue resulting in pneumothorax, pneumomediastinum, pneumoperitoneum, and subcutaneous emphysema
- Breath Stacking/Auto-Peep = occurs when air flow does not return to zero at end-exhalation. This is often seen in patients with COPD during spontaneous breathing.
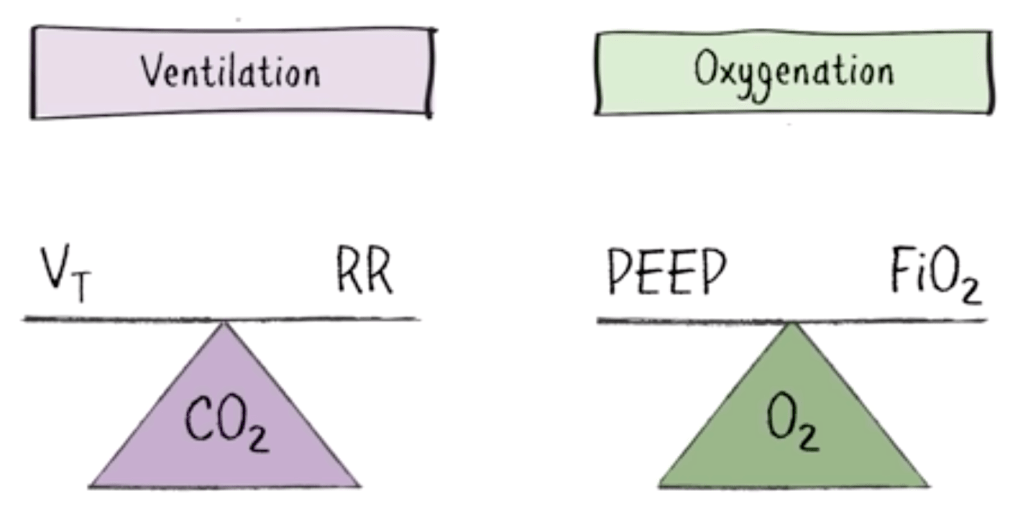
BASICS:
- When ventilation is the issue (ex, hypercapnia in patient with COPD or sepsis), consider changing the:
- Respiratory rate- RR has an inverse relationship with CO2. Increasing RR decreases your CO2 and vice versa
- Tidal volume
- When oxygenation is the underlying problem, change either
- PEEP- increasing PEEP recruits more alveoli but also increases risk of barotrauma
- FiO2
Ventilator Settings Most Commonly Used/Changed:
TIDAL VOLUME: Remember this is based on HEIGHT not weight, typically 6ml/kg

Ventilation Strategies:
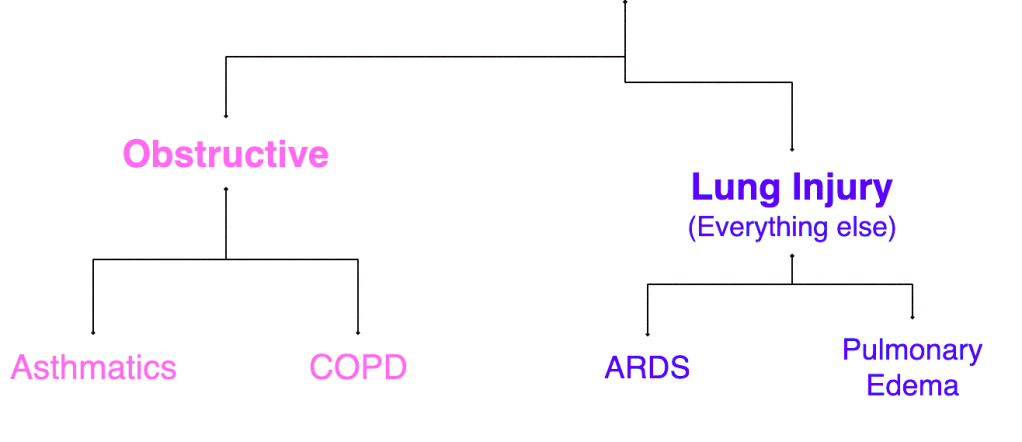
2 Types:
1. Obstructive: includes your asthmatics and COPDers
– remember the underlying dysfunction here is that patients are UNABLE to exhale placing them at risk for air-trapping
2. Lung Injury: includes everything else
Ventilating those with LUNG INJURIES
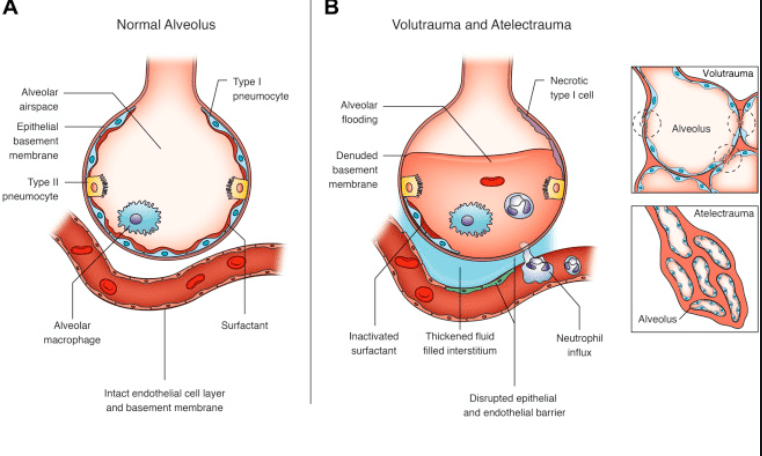
When the goal is to prevent further lung injury, barotrauma can be reduced with a low tidal volume and a higher PEEP.
WHAT CAUSES LUNG INJURY?
- OVERDISTENSION- occurs as a result of increased TV
- ATELECTRAUMA- Not enough PEEP.
- Every time alveoli collapse and re-expand, it exposes the alveoli to a shearing stress causing damage to alveolar wall
Ventilating those with OBSTRUCTIVE PATHOLOGIES
Goal = maximize expiratory time
Quick pathophysiology review: “COPD is a type of obstructive lung disease in which chronic, incompletely reversible poor airflow (airflow limitation) and inability to breathe out fully (air trapping) exist. The poor airflow is the result of breakdown of lung tissue and small airways disease known as obstructive bronchiolitis”
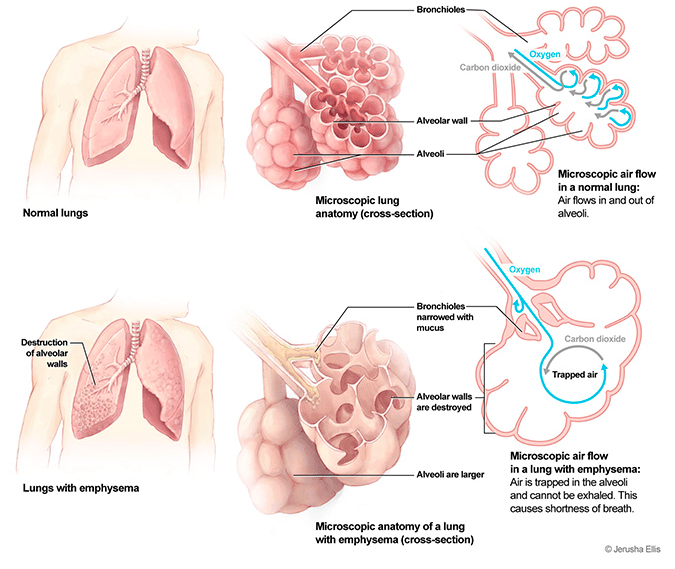
HOW?
- Decrease RR- This allows the patient to have time to exhale completely. Otherwise the vent will deliver another breath before the patient has exhaled completely leading to auto-PEEP or air- trapping/breath stacking
- Increase Inhale:Exhale (I:E) ratio (1:3 or even up to 1:4)
- High inspiratory flow rate- gets the air in faster so patient has more time to exhale
- Maintain PPlat < 30 cm H2O
- Permissive hypercapnia to avoid breath stacking
COMMON VENT ALARMS TO TROUBLESHOOT
Hypoxia
Go see the patient- make sure vent is connected
- Vitals/ETCO2- Check BP and assess perfusion. Is this oxygenation issue or is the patient not perfusing?
- Auscultate: Did the ETT shift or has a pneumothorax developed? A chest x-ray can help assess possible etiology
When assessing a patient that continues to be hypoxic, remember the acronym DOPES
D- displacement of ETT
O- obstruction of ETT (mucus plug)
P- pneumothorax, PE, pulmonary edema
E- Equipment, make sure vent is connected and functioning appropriately
S- Stacking of breaths
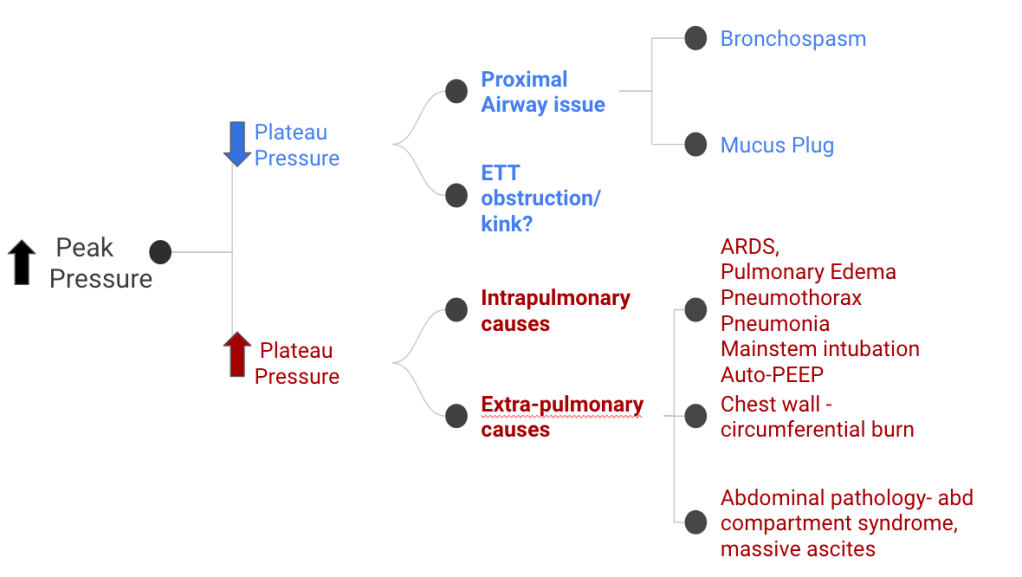
Elevated Peak Pressures
This indicates there is an elevated pressure somewhere between ETT and alveoli
Check plateau pressures- this will tell you if pressures are affected at the alveolar level. This value simply reflects the pressure it takes to hold a given value inside the lungs and when too high, will cause barotrauma. This can be obtained by doing an inspiratory hold (Pplat should be <30)
Take home points:
- COPDers/asthmatics require more time to exhale due to their obstructive disease- set RR on lower end, increase I:E to 1:3 or even 1:4
- Don’t be afraid to disconnect the patient from the vent and bag while troubleshooting.
- Peak pressures alone are not helpful, and should always be compared to plateau pressure.
- Remember the mnemonic DOPES if a patient is hypoxic post intubation
- This is not all exclusive information. Some resources I recommend and used for this:
https://www.emrap.org/episode/icufundamentals1/ventilator
https://www.emra.org/emresident/article/demystifying_ventilator_alarms/
Owens, William. The Ventilator Book. First Draught Press, 2018.
Written by: Sumyyah Yousufi, DO, MBA
Peer Reviewed and Edited by: Michelle Malnoske, MD


You must be logged in to post a comment.