An 8-day-old female presents to the emergency department with productive cough and worsening discharge from the left eye for two days. The patient’s mother also reported nasal congestion, cough, and wheezing. The patient had recently been evaluated 1 day prior in an ED and diagnosed with left lacrimal duct obstruction. At that time, no purulent discharge was noted however mother states over the last 24 hours since evaluation the child has developed purulent discharge instead of scant watery discharge and has had trouble opening the L eye from the amount of crusting and drainage that she has observed. On exam, there is copious mucopurulent drainage from the left eye with conjunctivitis. Lung exam revealed diffuse coarse breath sounds but no resp distress. There are no signs of dacrocystitis on exam.

Picture above: erythema and edema can be seen covering the upper lid. Mucopurulent discharge observed between lids as well as diffuse yellow crust noted around the eye. Picture was taken just after wiping away discharge as it quickly began to reaccumulate (Picture taken with parental consent and parents consented to publication of picture).
Neonatal Conjunctivitis
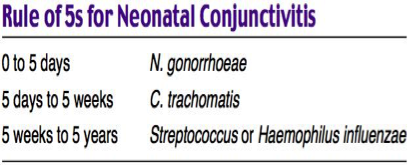
Neonatal conjunctivitis presents during the first month of life. It may either be aseptic or septic.
Chemical:
- Typically occurs on the first day of life
- Historically due to ocular prophylaxis with silver nitrate—now less common as erythromycin ointment is replacing silver nitrate
- Treatment is not necessary, however artificial tears may ease discomfort
Gonococcal
- Peaks at days 3-5 after birth
- Clinical
- Purulent discharge
- Profuse swelling and involvement of eyelid
- Corneal involvement
- Complications
- Corneal ulcer
- Blindness
- Disseminated disease may present as sepsis, arthritis, or meningitis
- Treatment
- Admission is required
- Given risk for disseminated disease, a complete neonatal rule out sepsis workup should be completed
- Topical therapy is not adequate for treatment. IV therapy with cefotaxime is needed.
Chlamydia
- Peaks at 1 week to 1 month after birth
- Clinical
- Mild swelling with watery discharge. Can also be mucopurulent
- Discharge can become bloody as the conjunctivae may be very friable
- Eyelid swelling
- Chemosis
- Pseudomembrane
- Mild swelling with watery discharge. Can also be mucopurulent
- Complications
- One-third of patients develop pneumonia
- Treatment
- Treatment should be initiated based on a positive diagnostic test
- Both ocular and nasopharyngeal swabs should be obtained
- Oral erythromycin (50 mg/kg/d divided QID) for 14 days
- Erythromycin is associated with pyloric stenosis in infants less than 2 weeks
- Children need to be monitored post abx for development of pyloric stenosis
- Topical therapy is not adequate
- Admission is not required if there is no complications/systemic disease
- Treatment should be initiated based on a positive diagnostic test
Herpetic
- Peaks at 6-14 days of life
- Clinical
- Excessive watering of the eye
- Conjunctival erythema
- Periorbital skin vesicles may or may not be present at the time of presentation
- Complications
- HSV keratoconjunctivitis may progress to cataracts and chorioretinitis and result in permanent vision impairment
- Disseminated disease
- Treatment
- 60 mg/kg/day IV divided TID for 14-21 days
Strep/Staph
- Peaks at 5 weeks to 5 years
- The most commonly identified organisms include staphylococcus aureus, streptococcus pneumoniae, streptococcus viridans, and staphylococcus epidermidis, which make up 30-50% of all cases neonatal conjunctivitis
- Clinical
- Purulent discharge at the lid margins and in the corners of the eye
- Treatment
- Erythromycin 0.5% ophthalmic ointment ½ inch (1.25cm) 4-6 times daily for 5-7 days
Case Conclusion:
Given the time course of her conjunctivitis and the child’s age, gonorrhea and chlamydia were a concern as it had became mucopurulent. Given the cough, a CXR was obtained which showed bilateral opacities throughout both lungs concerning for pneumonia. RSV and influenza antigens were negative. Eye culture including gram stain was obtained. Given the pneumonia in a neonate and concern for possible disseminated bacterial infection, a complete rule out sepsis workup was obtained including a lumbar puncture. Ampicillin and gentamicin were started after consultation with pediatrics. It was recommened to hold of on erythromycin for treatment of possible chlamydia initially.
The patient was admitted with a presumptive diagnosis of chlamydia conjunctivitis complicated by chlamydia pneumonia. CSF studies were negative. HSV PCR was negative. Eye culture was positive for streptococcus pneumonia but negative for both gonorrhea and chlamydia. The patient continued to improve and the discharge from her eye resolved. The patient was eventually diagnosed with bacterial conjunctivitis and streptococcus pneumonia.

