A 23 y.o male presents with worsening sore throat, dysphagia, and cough over the last 3 days. On exam, patient is in no acute distress but is tachycardic. Patient is able to speak in full sentences, has no stridor at rest, and is handling secretions. The patient’s oropharynx has notable erythema and swelling in the left peritonsillar area with some mild uvular deviation.
Peritonsillar abscess
Diagnosis:
The diagnosis of PTA can usually be made clinically without laboratory data or imaging in the patient with medial displacement of the tonsil and deviation of the uvula. Traditionally CT was used to confirm diagnosis if needed or if there was concern for spreading deep space infection or mass effect on the airway. Recently, ultrasound has been used to confirm the diagnosis and characterize the fluid collection as it is rapid, can be done at the bedside, and does not expose the patient to radiation.

Above is an image of a PTA using an endocavitary probe. Bedside ultrasound allows us to see the depth of the abscess, location of the abscess in the oropharynx to optimize needle insertion site, and if there are loculations. In the above image, you can see a hypoechoic fluid collection that extends down to about 2.5cm with loculations.
Drainage Tips:
Definitive treatment for a PTA is drainage, however anatomy needs to be highly considered when draining since important structures surround the area of infection such as the carotid artery and jugular vein.
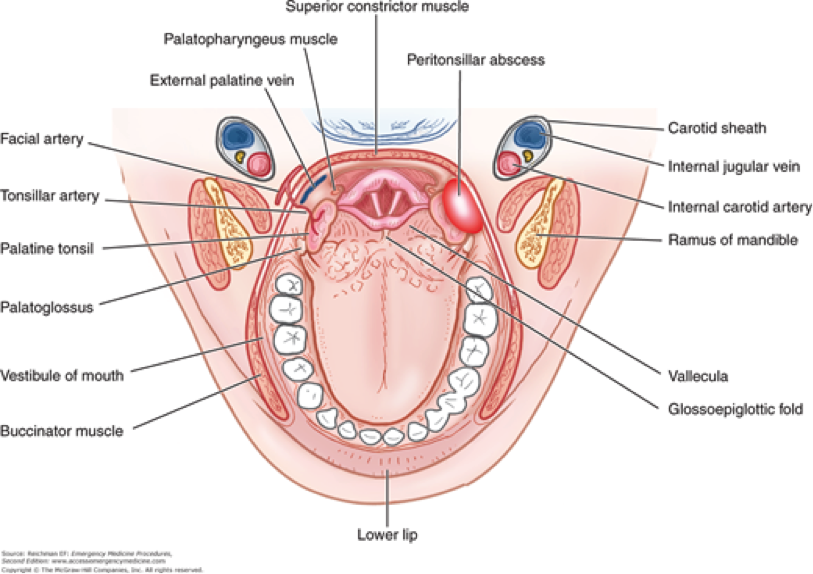
In order to avoid these structures, take the cap off your 18 gauge needle and cut the distal tip of the cap about 1cm back. After cutting the cap, place it back on the needle and this will prevent your needle from penetrating deeper than 1cm and will prevent you from accidentally puncturing the deeper vascular structures.

In terms of needles, a larger caliber needle such as 18g is preferable. If you find that your syringe is obstructing your view, you can consider using an 18g spinal needle instead so that the syringe remains out of the patient’s mouth.
In terms of anesthesia, a liberal topical application of your choice tends to be sufficient. We have benzocaine spray at our facility and we have found that topical application tends to be sufficient for needle aspiration and local infiltration is unnecessary.
A technique for maximizing view, moving the tongue, and illuminating the area is to use a laryngoscope. A cooperative patient can hold the laryngoscope with one hand and suction with the other which gives them a sense of control of the procedure and allows them to suction exudate and blood as it extrudes through the needle puncture of the abscess.

Case Resolution:
During drainage, about 6cc of purulent material was able to be aspirated. Post procedure patient had near immediate relief of pain. He was observed in the ED and his tachycardia resolved and he was able to tolerate PO. Patient was discharged on Augmentin.

Take Home Points:
- Ultrasound can be used as a quick bedside test to both confirm and characterize the abscess
- Be aware of the structures that lie deep to the peritonsillar area
- Cutting the cap of the needle and using a laryngoscope during the procedure are just a couple of ways to improve safety and visualization
- As needle aspiration is performed rather than incision and drainage in the ED, antibiotics and close return precautions are required

Great article- make sure the cap is adherent to the needle so it doesn’t drop in the airway
LikeLike