A 75 year-old male with a past medical history of coronary artery disease, hypertension, and hyperlipidemia presents to the Emergency Department via EMS for concern of altered mental status. His wife is present at the bedside and states that he been becoming progressively more confused over the past 2 days. Prior to this episode, he was a high functioning individual without any major issues. Besides the confusion, the patient does endorse some dizziness; however is unable to give any further details due to his confusion. His wife denies any other reported symptoms, including chest pain, dyspnea, fever, chills, nausea, vomiting, diarrhea, abdominal pain, back pain, dysuria, hematuria, or headache.
You examine the patient and find him to be alert and oriented to self only. His pupils are equal and reactive. Neck is supple without evidence of meningismus. Lungs are clear. The heart is bradycardic with a regular rhythm and no murmurs, rubs, or gallops. Abdomen is soft and non-tender. There is no peripheral edema. He is grossly neurologically intact and able to move all 4 extremities.
As the nurse is getting him hooked up to the monitor, you note his heart rate is 35, blood pressure is 80/60, with normal oxygen saturation, temperature, and respirations. You immediately obtain an EKG which is shown below.
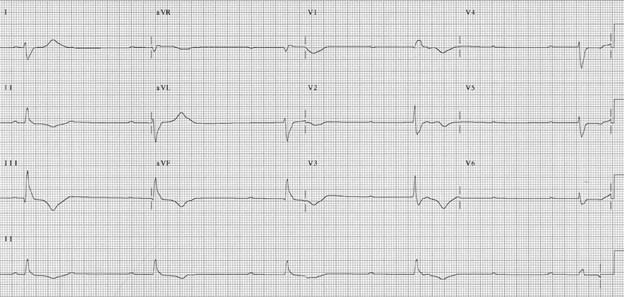
After reviewing the EKG, you quickly ascertain that your patient is in symptomatic complete heart block and will require immediate intervention. You set up transcutaneous pacing at a rate of 60 beats per minute and the nurse obtains some blood testing. Over the next several minutes, his blood pressure improves to 100/70 and his wife thinks that his confusion is beginning to improve. You then go and speak with cardiology, and they agree with your assessment that the patient is in complete heart block and will require hospital admission and a permanent pacemaker. In the meantime, they ask you to place an intravenous pacemaker and admit the patient to the ICU.
Pathophysiology:
Complete (3rd degree) heart block is defined as the complete dissociation of the atria and ventricles. It is caused by severe and permanent damage to the conducting system of the heart, either the AV node or the His-Purkinje system. Impulses from the SA node do not reach the ventricles and the ventricular rhythm is maintained by a junctional rhythm or ventricular escape rhythm, resulting in P waves and QRS complexes occurring at 2 separate rates, as seen in the EKG below. This rhythm is inherently unstable and can result in sudden cardiac death. As seen in the case above, it requires transcutaneous and/or transvenous pacing, ICU admission, and placement of a permanent pacemaker.
In addition to complete heart block, there are other types which are briefly highlighted below.
The mildest type of heart block is first degree, which is defined as a prolonged PR interval >200ms. This is a benign finding as there are no sequela of first degree AV block and no risk of progression to more advanced forms of AV block.

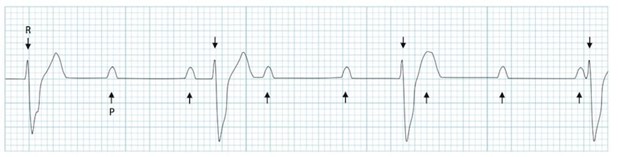
The next type of heart block is second degree, which is divided into two subtypes, Mobitz I (Wenckebach) and Mobitz II (Non-Wenckebach). Both types involve dropped QRS beats; however the difference lies in the PR interval. In Mobitz I, the PR interval will progressively lengthen until a beat is dropped. This is caused by a reversible defect in the AV node, such as an inferior MI or AV nodal blocking agents (beta blockers, calcium channel blockers, or digoxin). In Mobitz II, the PR interval does not change from beat to beat and a beat will randomly drop. This is caused by a sudden and irreversible damage to the His-Purkinje system, such as autoimmune disease, anterior MI, and cardiac surgery near the ventricular septum. Mobitz I does not carry much clinical significance and is usually benign; however Mobitz II has a high chance of progressing to complete heart block. Thus, any patient in the ED found to have a Mobitz II block should be admitted for telemetry monitoring and pacemaker placement.

Mobitz I. Note the progressively lengthening PR interval until a beat is dropped.

Mobitz II. Note the stable PR interval with 2 sudden dropped beats.
Case conclusion: The patient underwent successful permanent pacemaker placement the following day and was discharged back home, where he resumed his usual activities.
Written By: Sean Horoho, MD
Reviewed By: Zoran Kvrgic, MD and Jeremy Lux, DO
Posted By: Valerie Hardoon, MD
References
Life in the Fast Lane: http://www.litfl.com
https://fineartamerica.com/featured/heartbeat-madame-memento.html?product=art-print

