Patient case
This is a case involving a 34-year-old woman who has presented to the emergency department with a sudden and rapid onset of painless monocular vision loss. Last well known well was 2 hours ago. The patient’s medical history includes hypertension, atrial fibrillation, hyperlipidemia, diabetes, lupus, and a history of tobacco use. She reported waking up this morning and experiencing this new and unexpected vision loss. Currently, she is taking atenolol for her hypertension, Xarelto for anticoagulation and metoprolol for rate control of her atrial fibrillation, atorvastatin for hyperlipidemia, Ozempic for diabetes management. It’s important to note that she has not been consistently following up with her lupus medication due to financial constraints and limited access to a rheumatologist. Additionally, the patient has been smoking one pack of cigarettes per day for the past 10 years. Patient denies recreational drug use. No further medical problems noted. After a fundoscopic exam, it was observed that this patient has CRAO. On fundoscopic exam noticed cherry red fovea with a pale retina. Patient received fibrinolytic therapy with the consultation of ophthalmology, admitted to medicine where ophthalmology and rheumatology were able to further manage the care of the patient.
Background
Central retinal artery occlusion (CRAO) is an occlusion of the central retinal artery leading to painless vision loss. This can be thought of as an acute ischemic stroke within the central retinal artery. The timeline is important with CRAO. The time between the initial onset to provider is important because retinal tissue can be preserved with earlier intervention. This is also a similar feature or rather analogous to an ischemic stroke.
It is important to have an appreciation for the inner retina which is composed of retinal nerve fiber layer, ganglion cells, inner plexiform layers which is supplied by the central retinal artery and collateral branches. It is important to note that individuals that do have collateral circulation ( posterior ciliary circulation) vision may return to normal or close to normal. It is classic to see cherry red spot on fovea given the collateral circulation. You may also see pale retina due to the occlusive pathology.
There are two major categories of CRAO which consist of Arthritic and Nonarteritic CRAO. Arthritic CRAO involves an inflammatory cascade causing occlusion of arteries. This includes giant cell arthritis, lupus and various vascular inflammatory syndrome diseases and disorders. Nonarthritic CRAO is when thrombosis is the major cause usually secondary to endothelial cell damage (diabetes, hyperlipidemia or hypertension) or cardiac embolism.
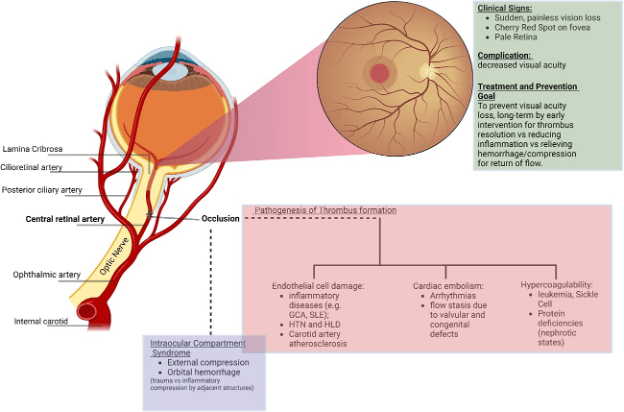
Figure 1.
Demonstrates pathological causes of CRAO. The internal carotid artery give rise to the ophthalmic artery which branches into the central retinal artery and collaterals.
Clinical Presentation
Painless monocular vision loss with rapid and sudden onset is classic in the presenting case. You must also be aware of other signs of CRAO including steady loss of eyesight in one eve over a few weeks. It is important to gather good history of the patient and family history of the patient.
Diagnosis
It is important to complete an fundoscopic exam on these patients. Close to 90% of patients will show a cherry red spot on fundoscopy. Other findings will be optic disk edema, pallor and or segmentation of the arterioles.

Figure 2. Cherry red spot with central retinal artery occlusion
Differential Diagnosis
It is important to have a vast differential diagnostic list. You must think of autoimmune vascular diseases given that CRAO can be arthritic. This includes giant cell arteritis, lupus, small medium and large vascular diseases. Also during your workup you should include acute angle closed glaucoma, globe rupture, vitreous hemorrhage, retinal detachment, psychiatric causes.
Management
When a patient presents with monocular vision loss, and a diagnosis of Central Retinal Artery Occlusion (CRAO) has been established, several therapeutic approaches should be considered. These options aim to improve the ocular perfusion and address the underlying causes:
- Intraocular Pressure Reduction: Initiate treatment with intraocular pressure-lowering medications, such as beta-blockers and alpha agonists. This intervention is critical for reducing intraocular pressure and enhancing vascular perfusion.
- Intravenous Fibrinolytic Therapy: For patients within the 4.5-hour window of symptom onset, consider the administration of intravenous fibrinolytic agents. This approach can help in restoring retinal blood flow and improving visual outcomes.
- Management of Underlying Autoimmune Diseases: If CRAO is secondary to an underlying vascular autoimmune disease, you will need to address the autoimmune condition as part of the management plan. This may involve immunosuppressive agents or disease-modifying drugs and a rhumatologst consultation.
- Consultation : Consultation with an ophthalmologist is important to optimize treatment strategies and long-term care.
Written by: Manzy Byrd DO, MS
Reviewed by: Jeremy Lux, DO, FACEP, FAAEM, Zoran Kvrgic, MD
References by:
Hellmich B, Agueda A, Monti S, Buttgereit F, De Boysson H, Brouwer E, Cassie R, Cid MC, Dasgupta B, Dejaco C, et al. 2018 Update of the EULAR recommendations for the management of large vessel vasculitis. Ann Rheum Dis. 2020; 79:19‐30. https://doi.org/10.1136/annrheumdis‐2019‐215672CrossrefMedlineGoogle Scholar
Dagra A. Created with Biorender. 2023.Google Scholar
Dollery CT, Bulpitt CJ, Kohner EM. Oxygen supply to the retina from the retinal and choroidal circulations at normal and increased arterial oxygen tensions. Invest Ophthalmol. 1969; 8:588‐594.Google Scholar

