Case: A 70 year-old female with a past medical history of CAD and Type 2 Diabetes presents to the ED with generalized weakness, fatigue, and confusion for the past week. Her caretaker denies any inciting events and notes a progressive decline in her health during this time. She checked the patient’s blood sugar at home this morning and her meter read “high,” which is what made them seek care. Review of systems is positive for abdominal pain, nausea, and urinary frequency. Upon exam, the patient is awake, alert, and oriented to person and place, but not time. Vitals are unremarkable except for a heart rate of 110. Oral mucosa are dry and the patient appears dehydrated. The remainder of the exam is unremarkable. You ask the patient’s nurse to obtain a fingerstick glucose, some basic labs, and start a liter bag of normal saline while you formulate your plan.
Physician: You are considering a wide differential in this patient given her age and co-morbidities; however given her elevated blood sugar reading, diabetic complications are at the top of your list. Diabetic ketoacidosis (DKA) and Hyperosmolar hyperglycemic state (HHS) are two things that come to mind and you begin to think about the differences between these conditions. This reminds you that you need to obtain a CBC, CMP, VBG, lactic acid, blood cultures, serum ketones, and serum osmolality to further differentiate these conditions. Given the patient’s urinary symptoms, you also decide to obtain a urinalysis as underlying infection can often trigger DKA and HHS. As you are doing further research on DKA and HHS, you run across the diagnostic criteria which can distinguish between these conditions, as well as some information about different conditions that can precipitate HHS.

Fig. 1: Diagnostic criteria for DKA and HHS. From Tintinalli’s 9e

Fig. 2: Drugs that can cause HHS. From Tintinalli’s 9e
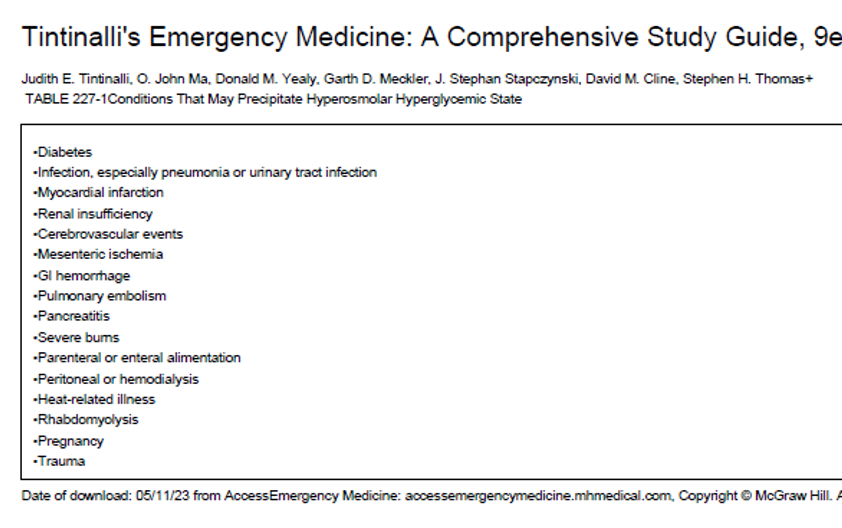
Fig. 3: Medical conditions which can cause HHS. From Tintinalli’s 9e
Case: You review the blood work and it is notable for a blood glucose of 650, sodium of 150, potassium 5.5, BUN 45, Creatine 2.2, serum osmolality of 330, pH of 7.35, anion gap of 11, lactate of 3.2, and negative serum ketones. Urinalysis is notable for a UTI. Blood cultures are still pending. Upon your reevaluation, the patient remains A/O x2 and tachycardic, with the remainder of her exam unchanged from her initial presentation. Due to the hypernatremia, you ask the nurse to stop the normal saline and switch to lactated ringers. You also order a dose of piperacillin-tazobactam for broad-spectrum coverage in this patient who is septic. Her blood pressure remains stable and she does not require pressors at this time. At this point, you are suspecting HHS which was likely precipitated by a UTI that has now become urosepsis. You ask the patient’s nurse to hang a second liter of LR once the first liter finishes to give a full 30cc/kg bolus to meet sepsis criteria and ask her to recheck the lactate following the administration of the second liter of fluids. You wonder if this patient should be given insulin to correct her profound hyperglycemia.
Physician: You review the treatment recommendations for HHS and find the algorithm as seen below. You have correctly started with fluids to replace the volume losses and realize that this patient will require more fluids than you would be able to replace in the ED. You then see that persistently elevated glucose despite fluid resuscitation requires IV insulin dosed at 0.1 units/kg/hr, assuming that the potassium is not low. You double check the patient’s potassium, note it to be 5.5, and see that you can safely start an insulin drip, with careful monitoring of the potassium. You decide that you will check hourly BMPs until the patient leaves the department.
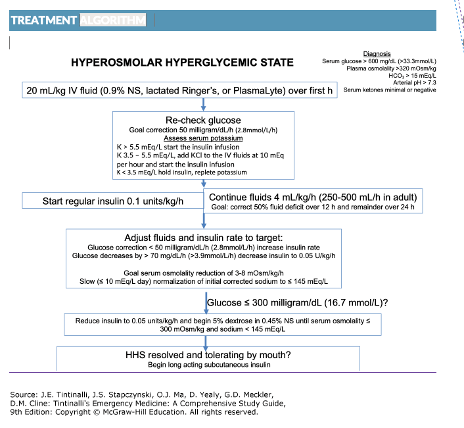
Fig. 4: HHS Treatment Algorithm. From Tintinalli’s 9e
Case: After asking the nurse to start IV insulin at 0.1 units/kg/hr and to check hourly BMPs, you call the ICU to admit the patient for further monitoring and treatment. She thanks you and her nurse for taking excellent care of her.
Written By: Sean Horoho, MD
Reviewed By: Stevley Koshy, DO
References
Tintinalli’s Emergency Medicine, A Comprehensive Study Guide, 9th Edition


You must be logged in to post a comment.