History of Presenting Illness
A 5-year-old boy was brought to the emergency department with severe abdominal pain, fever, vomiting, rebound tenderness, and guarding. His symptoms strongly indicated acute appendicitis. The pain began just a day ago, initially accompanied by fever and localized to the right lower quadrant. Considering the child’s low-grade fever, vomiting, anorexia, and tenderness in the right lower quadrant, his risk for appendicitis was moderate. The pain worsened with activities such as walking, jumping, and coughing. Based on the Alvarado score of 5, appendicitis was suspected. A complete blood count revealed a leukocytosis of 17.2, and an ultrasound of the appendix raised concerns for appendicitis. The patient received 1 gram of ceftriaxone and 500 mg of metronidazole. Fluids were administered, and a consultation with the general surgery team was requested for urgent surgical intervention.
Imaging


Fig 2: Demonstrating normal appendix vs inflamed appendix for ultrasound findings
Introduction
Appendicitis occurs when the lumen of the appendix becomes obstructed, leading to inflammation. This obstruction can arise from various sources, including the presence of fecal material, parasites, or an enlarged lymphoid follicle within the epithelial lining of the appendix. These factors can impede the normal flow of contents through the appendix, resulting in a buildup of pressure and subsequent inflammation.
In addition to mechanical obstructions, another contributing factor to the development of appendicitis is the overgrowth of bacteria within the lumen. This bacterial overgrowth is often secondary to an infection, commonly caused by Escherichia coli. The presence of these bacteria can further exacerbate the inflammatory response within the appendix, leading to the characteristic symptoms associated with appendicitis.
It’s important to note that while these are recognized causes of appendicitis, the exact trigger for the initial obstruction or bacterial overgrowth may vary from person to person. Various factors, such as dietary habits, genetic predisposition, and overall gut health, can influence an individual’s susceptibility to developing appendicitis.
Clinical Manifestations
In cases of appendicitis, it is often observed that patients experience anorexia (loss of appetite) and periumbilical pain, which then migrates to the right lower quadrant within the initial 24 hours. Subsequently, fever commonly develops within 24 to 48 hours after the onset of symptoms. However, it is important to note that the manifestation of these symptoms may vary depending on the age of the child, particularly between neonates and young children.
In neonates, distinctive signs of appendicitis typically include abdominal distension and vomiting. These symptoms may be indicative of the condition and prompt further investigation to confirm the diagnosis. On the other hand, in children aged 1 to 5 years, the predominant symptoms of appendicitis are often abdominal pain accompanied by fever. Recognizing these specific symptom patterns aids in establishing an accurate diagnosis and initiating appropriate management.
Clinical Diagnosis: Appendicitis is primarily a clinical diagnosis, meaning that healthcare professionals rely on the patient’s symptoms, physical examination findings, and medical history to assess the likelihood of appendicitis. Common clinical manifestations include abdominal pain, fever, nausea, vomiting, and tenderness in the right lower quadrant of the abdomen. Other signs, such as rebound tenderness and guarding, may also be present. The healthcare provider will carefully evaluate these factors to determine the likelihood of appendicitis.
Imaging Studies: Ultrasound is often the initial imaging modality used to evaluate appendicitis. It helps visualize the appendix and surrounding structures, assisting in the detection of inflammation, swelling, or the presence of an abscess. However, if the ultrasound findings are inconclusive or the clinical suspicion remains high despite a negative ultrasound, a computed tomography (CT) scan may be considered. CT scans provide detailed cross-sectional images, offering a more comprehensive evaluation of the appendix and potential complications.
Complete Blood Count (CBC): A CBC is a routine blood test that measures various components of the blood, including the number of white blood cells (WBCs). In cases of appendicitis, an elevated WBC count, known as leukocytosis, is often observed. This can indicate an inflammatory response in the body, supporting the diagnosis of appendicitis. However, it is important to note that leukocytosis can also be present in other conditions, and its absence does not rule out appendicitis.
Management
Antibiotics: In the presence of acute appendicitis, antibiotics are often administered to help control the infection and prevent complications. Commonly used antibiotics include Ceftriaxone and Metronidazole, which provide broad-spectrum coverage against bacteria commonly associated with appendicitis. The specific choice of antibiotics may vary depending on factors such as local antimicrobial resistance patterns and individual patient characteristics.
Fluid Administration: Adequate hydration is essential during the management of appendicitis. Intravenous fluids are typically administered to maintain hydration and electrolyte balance. Fluids help compensate for any fluid loss due to vomiting, decreased oral intake, or potential surgical interventions..
Pain Management and Fever Control: To alleviate pain and discomfort associated with appendicitis, analgesic medications are often prescribed. Nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids may be used to provide pain relief. Additionally, antipyretic medications such as acetaminophen may be administered to reduce fever, if present
Surgical Intervention: The definitive treatment for acute appendicitis is the surgical removal of the inflamed appendix, known as an appendectomy. This can be performed through an open surgical approach or using minimally invasive techniques such as laparoscopic appendectomy.
Disposition
- Consult Surgical services
- Admit to hospital
Written By: Manzy Byrd MD
Reviewed By: Stevely Koshy MD, Zoran Kvrgic MD
References:
- Uptodate: Management of Acute Appendicitis
- Radiology assistant: Management of Acute Appendicitis
- Rosen’s Emergency Medicine: Concepts and Clinical Practice: 2-Volume Set 10th Editionby Ron Walls MD (Author), Robert Hockberger MD (Author), Marianne Gausche-Hill MD FACEP FAAP (Author), Timothy B. Erickson MD FACEP FACMT FAACT (Author), Susan R. Wilcox MD (Author)
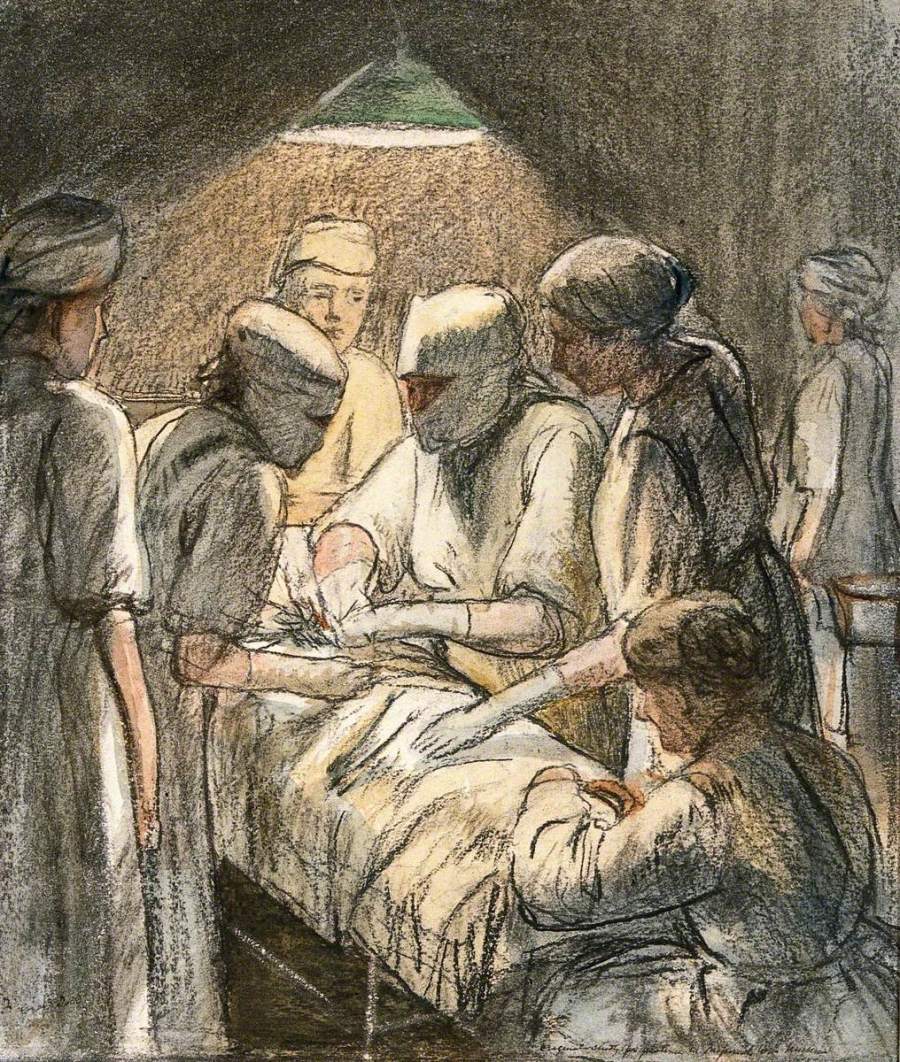
- https://artuk.org/discover/artworks/an-operation-for-appendicitis-at-the-military-hospital-endell-street-london-240777

You must be logged in to post a comment.