19-month-old female presents to the ED for evaluation of shortness of breath and wheezing, seen in walk in clinic just prior to arrival and noted to be 87% on room air. She has been eating and drinking slightly less but has had adequate urine output and has had no noted fevers at home. In arrival to triage patient is calm and is noted to be saturating at 93% on RA. On examination patient is interactive, does fuss when examined and this is noted to decrease her SPO2 to 87% on RA. Her lungs have rhonchi throughout, and her breathing is noted to be labored with some mild subcostal retractions. Notably, the patient was admitted directly to the hospital 18 days prior to presentation for hypoxia that was secondary to a rhinovirus infection. She did not receive a chest x-ray at that time.
Patient was placed on 2L O2 by nasal cannula and her SpO2 increased to 97% at rest, she would stay at this saturation unless made to be upset by staff. A chest x-ray was ordered and COVID/RSV/Flu swab was run. The swab came back negative and her chest x-ray showed “Boot-shaped cardiac morphology, often described in the setting of Tetralogy of Fallot. Correlation with echocardiography and patient history might be considered. Mildly to moderately increased perihilar markings, but no focal consolidation or pleural effusion.”
Epidemiology and Pathophysiology of Tetralogy of Fallot
The prevalence of TOF in the United States is approximately 4 to 5 per 10,000 live births. This defect accounts for approximately 7 to 10 percent of cases of congenital heart disease and is one of the most common congenital heart lesions requiring intervention in the first year of life. TOF occurs equally in males and females. There is no identified recessive/dominate inheritance pattern, it is a result of a mutation. There is a strong association with Down Syndrome individuals.
It is caused by misalignment of the endocardial cushion during embryonic development. This leads to the characteristic 4 findings in the tetralogy:
- Ventricular Septal Defect
- Most commonly a single large, malaligned subaortic defect located in the perimembranous region of the septum
- Right Ventricular Outflow Obstruction
- Often at multiple levels along the outflow tract
- Anterior and cephalad deviation of the infundibular septum results in subvalvar obstruction
- Hypertrophy of muscular bands in this region can further accentuate subvalvar obstruction
- Pulmonary valve annulus is usually hypoplastic, although, in some instances, it is of normal size
- Pulmonary valve itself is frequently bicuspid and stenotic
- Often at multiple levels along the outflow tract
- Overidding Aorta
- Aorta is displaced towards the right heart, which causes it to override the previously mentioned VSD
- Right Ventricular Hypertrophy
- The combination of the above factors leads to increased strain on the RV, causing hypertrophy
These defects lead to cyanosis of the newborn and a ductal dependency as the blood mixes from the right and left sides of the heart. As the blood is not able to escape the right ventricle to the lung, the only way for the blood to become oxygenated is to have it pass from the aorta through the ductus arteriosus into the pulmonary arteries. Despite this, the oxygenated and preoxygenated blood ends up mixing in the LV and Aorta and gets sent systemically. This causes the peripheral oxygen saturation to be low at baseline.
Clinical Features of Tetralogy of Fallot
The aforementioned mixing of deoxygenated blood can give babies with ToF a blue color at baseline, mean SpO2 concentration is 79% +/- 4% based on one study from Qiang Li et al. Most cases are diagnosed either before or shortly after birth due to this. It is possible for milder cases, especially if the RVOT is not fully obstructed to go undiagnosed until later in life.
Under certain conditions, such as stress from a systemic disease, the outflow tract obstruction can become worse, and patients will have ‘Tet’ spells. During these, they become rapidly cyanotic and bring their knees and arms towards their chest in order to increase preload to the heart, which helps to alleviate this obstruction. These occur primarily when the patient is agitated or upset. In our patient, we did not observe severe cyanosis, but her SpO2 was noted to decrease when she became upset.
On auscultation of the heart, you may hear a slight click at early systole due to extra blood entering a dilated aorta. There is also usually a harsh crescendo-decrescendo sound that is due to the RVOT obstruction.
Diagnostic Tools in the ED
Echocardiogram is the mainstay of noninvasive assessment of ToF. There are some characteristic features though that may show up on an x-ray and may be useful in evaluation in the ED.

The characteristic findings seen here are:
- Hyperinflated lungs
- Decreased pulmonary vasculature from lack of pressure through the pulmonary arteries
- The aorta is concave to the right due to its malposition
- There is a boot shape to the heart secondary to RV enlargement
EKG is another tool we often use in the ED that can be used to identify ToF with low sensitivity and specificity.

The findings that suggest ToF above are all indicative of right ventricular hypertrophy and right heart strain:
- Prominent p waves in V1
- Rightward axis deviation
- Prominent R wave in V1
Lastly, we can use bedside ECHO to try and evaluate some of the features of ToF.

Ventricular septal defect appearing as a gap between the two septums on parasternal long axis view.
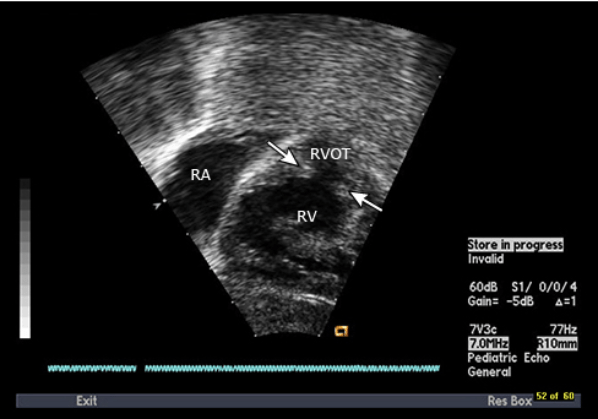
Pulmonary outflow tract obstruction seen as discontinuation of blood flow from the right ventricle

RV hypertrophy seen as enlargement of the RV when compared to the LV.
In our patient, she had an upturned heart with boot like shape, suggestive of ToF but did not have any of the other signs like lack of peripheral vascularity or hyperinflated lungs. We did do a bedside ultrasound and thought we witnessed some RV hypertrophy but were not able to find other parts of the heart to try and compare them to the above images to further evaluate ourselves. Since the patient was having intermittent episodes of hypoxia given her relatively normal chest x-ray, a decision was made to transfer to a tertiary facility for further evaluation.
Management of a Child with ToF in the ED
In our patient with a suspected minor viral URI to trigger her mild hypoxia, some slight nasal cannula O2 was all that was needed to bring her to normal O2 saturation. In general, with a patient who has a history of ToF when they arrive with normal disease process, they will also become slightly more hypoxic, necessitating supportive care in the manner of O2 supplementation and possibly fluids to help increase preload.
Summary and Conclusion
The vast majority of Tetralogy of Fallot will be diagnosed prior to a patient presenting to your ED. When they do, expect their already low SpO2 to dip even lower, even with mild illness. You should treat this as you would any other hypoxic child, keeping in mind your goal is high 70% to low 80%. If you have a child with hypoxia for an unexplained reason and is fairly young, keep ToF and other heart defects on your differential and use some of the above tools, (chest x-ray, EKG, bedside ECHO) to try and further evaluate for these conditions.
Written By: Maxwell Brown, DO
Peer Reviewed and Edited by: Stevely Koshy, DO
Sources:
- Li, Qiang, et al. “Pulse Oxygen Saturation Measured in Standing and Squatting Positions May Be Useful in Evaluating Tetralogy of Fallot.” The Heart Surgery Forum, vol. 12, no. 1, 2009, https://doi.org/10.1532/hsf98.20081110.


You must be logged in to post a comment.