Intro:
- Distal digital trauma is common and often associated with cosmetic and functional disturbances.
- Underlying lacerations are often masked by gross deformities of the nail and hematomas.
- Crush and blunt force injuries are usually the mechanisms involved with nail deformities and underlying nailbed injuries.
- Treatment can often necessitate nail removal based on clinical judgement and suspicion of underlying injuries.
- If the germinal matrix is intact, the nail will likely grow back, albeit rather slowly.
Anatomy:
- In order to better understand injuries and management, here are the highlights of the important anatomical regions which should be used to better describe the injuries.
Hyponychium: Distal nail fold
Eponychium: Proximal nail fold
Paronychium: Lateral nail folds
Cuticle: Extended portion of the eponychium which helps form a seal to promote nail growth.
Germinal Matrix: Responsible for nail formation. Located deeper than the eponychium.
Nail Bed: Directly below the nail plate. Highly vascular structure providing a base for the nail to grow
Nail Plate: The hard part of the nail which is made of keratin.
Subungual hematoma:
- Blunt crush injuries are often associated with a hematoma forming under the nail.
- It is important to consider fractures and evaluate for extensor tensor injury (Mallet finger)
- Causes a significant amount of pain due to the increased pressure from the accumulation of blood.
- Trephination is a simple but highly effective treatment for these conditions which involves forming a hole in the nail to release pressure.
- Successful trephination will result in blood oozing out of the hematoma.
- Only attempt for hematomas < 48 hours old as otherwise the blood will be clotted.
- Classical thinking involved nail removal for large hematomas to repair nailbed lacerations however there has been a recent change in thinking as this would introduce more trauma to a region which could heal well spontaneously.
- Trephination is often needed for hematomas >25% in size when compared to the nail, however can be attempted for smaller hematomas if there is discomfort.
- However newer studies have shown adequate healing in larger hematomas with trephination alone.
- Nail can stay in place if the paronychium is intact and no significant concern for lacerations.
- Equipment needed includes a cautery pen or sharp 18-gauge needle.
- Anesthesia isn’t necessary as the nail is insensate. Sensory nerves are present in the underlying nailbed.
- Apply gentle pressure with the electrocautery device to form a hole with the nail and blood begins to ooze out.
- Immediately remove the cautery device to prevent damaging the underlying nailbed.
- While it is more difficult, spinning a sharp needle with pressure on the nail over the hematoma will provide a similar outcome after penetrating the nail.
- Twist the needle like a drill.
- Do not use cautery for trephination of an acrylic nail to avoid starting a fire.

Nail removal:

- As noted, traditional thinking involved nail removal for large hematomas to repair nailbed lacerations however there has been a recent change in thinking as this would introduce more trauma to a region which could heal well spontaneously.
- If the nail is maintaining its structure and not grossly elevated, and the lateral folds are intact, the nail itself should provide a smooth barrier for any underlying minor lacerations to heal. The pressure from the intact nail will also help provide hemostasis. So for suspicion fo minor injuries with an intact nail, the nail does not need to be removed.
- In general, any malformed or displaced nails need to be removed.
- Use these steps to remove a nail
- Digital block for comfort.
- Lidocaine with epinephrine is perfectly acceptable despite classical thinking (Chowdhry et al, 2010).
- Using a hemostat, firmly grasp the nail.
- Using a lifting and turning motion, gently lift the nail from each side which should elevate it above the paronychial folds.
- With gentle outward pressure, the lifted nail should come off fairly easily.
- Acrylic nails can be removed by soaking in acetone.
- There are multiple ways to approach this including using acetone soaked gauze, bowl of acetone, or several acetone wipes and wrapping the nail.
- It can take 20-30 minutes for the adhesive to be dissolved.
- Gently pry off the nail when loose.
Laceration Repair:
- All lacerations should be evaluated thoroughly for underlying tendon injuries.
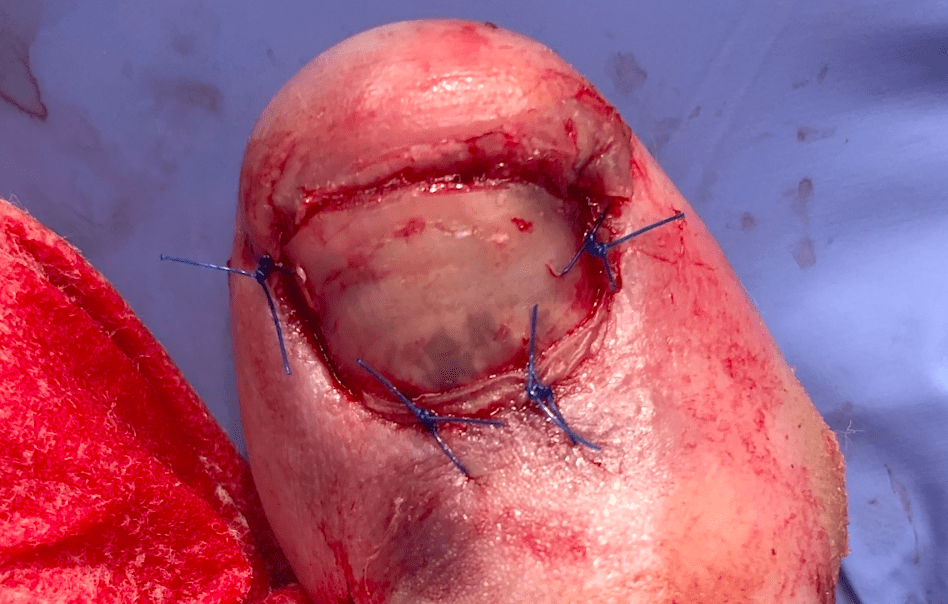
- After the nail is removed, irrigate thoroughly and evaluate the wound.
- Create a bloodless field by applying a tourniquet on the digit proximally.
- In general, germinal matrix injuries could lead to permanent nail deformities and should be repaired and be followed by a hand/foot specialist.
- The main goal of nail bed laceration repair is to form a flat surface to be the base for the nail to grow over.
- Use absorbable thin sutures such as 6-0 fast absorbing sutures for repairing deeper lacerations.
- Skin adhesives (dermabond) have been equally effective in nail bed laceration repair and is much faster.
- Adhesives will only work if the nailbed is dry and wound is well approximated.
- In order to maintain the shape of the nailbed and facilitate new nail growth, the removed nail can be sutured back on the digit to cover the nail bed.
- Use non-absorbable suture and have them follow up for removal in 2 weeks which gives adequate time for the nailbed to heal and the old nail will fall off.
- Preload the needle and suture through the nail which will avoid deeper punctures when re-attaching the nail.
- This is more cosmetically pleasing for the patient as well.
- If the nail was not salvageable, use petroleum jelly soaked gauze and aluminum foil to accomplish the same goal.
- Newer literature has shown normal healing of the nailbed even without any covering, however patient’s find a salvaged nail more aesthetically pleasing.
- There are also still concerns of scarring from the lacerations leading to deformities for the new nail.
Tuft Fracture:

- Rates of osteomyelitis in adults with open distal phalanx fractures has been very low.
- There is mixed evidence currently regarding antibiotic use in adults with open distal phalanx fractures.
- Regardless of antibiotic use, the wound should undergo copious irrigation under a digital block.
- The thought is that since the area is highly vascular and can be irrigated very well under a digital block, the risk of infection is far lower.
- Seymour fractures are pediatric Salter Harris I/II open fractures.
- These can have growth deformities and warrant an Ortho/Hand consult.
- Antibiotics should definitely be used for pediatric Seymour fractures with acceptable coverage being a 7 day course of cephalexin.
- Distal phalanx fractures are often managed non-operatively
- Apply a finger splint and instruct to leave this on for 2-3 weeks.
- Provide orthopedic follow-up for re-evaluation and decisive management.

Summary:
- Digital blocks when done appropriately should provide adequate analgesia.
- Lidocaine with epinephrine is perfectly acceptable despite the old dogma of not using epinephrine for digital blocks.
- Multiple retrospective studies showed no complications.
- Trephinate sublingual hematoma for release of pressure and effect seen by release of blood
- Repair nail bed lacerations with absorbable suture and skin adhesives.
- Use non-absorbable sutures to reapply the salvaged nail or gauze and petroleum jelly with aluminum foil to maintain the shape and integrity of underlying nailbed.
- If the laceration is associated with a distal phalanx fracture, immobilize for 2-3 weeks.
- Complex repair or those involving the germinal matrix should be followed by a hand/foot specialist.
Written by: Akhilesh Dakwale, MD
Edited and peer reviewed by: Dylan Kellogg, MD
References:
- EMRAP
- Uptodate
- https://www.aocd.org/page/SubungualHematoma
- Bharathi, R Ravindra, and Babu Bajantri. “Nail bed injuries and deformities of nail.” Indian journal of plastic surgery : official publication of the Association of Plastic Surgeons of India vol. 44,2 (2011): 197-202. doi:10.4103/0970-0358.85340
- Chowdhry S, Seidenstricker L, Cooney DS, Hazani R, Wilhelmi BJ. Do not use epinephrine in digital blocks: myth or truth? Part II. A retrospective review of 1111 cases. Plast Reconstr Surg. 2010 Dec;126(6):2031-2034. doi: 10.1097/PRS.0b013e3181f44486. PMID: 20697319.


You must be logged in to post a comment.