A 56 y.o m with a hx of HTN and tobacco use presents for chest pain. The patient states that today while mowing his lawn he started getting midsternal chest pain. He has never had this before. It is not pleuritic or positional, and it radiates to his jaw and L arm. EMS arrived and administered nitroglycerin and aspirin, and by the time the patient arrives to the ER he states his pain is completely gone.
His vital signs are unremarkable without tachycardia, hypotension, or hypoxia, and his full physical exam has no abnormalities. You obtain an initial EKG:

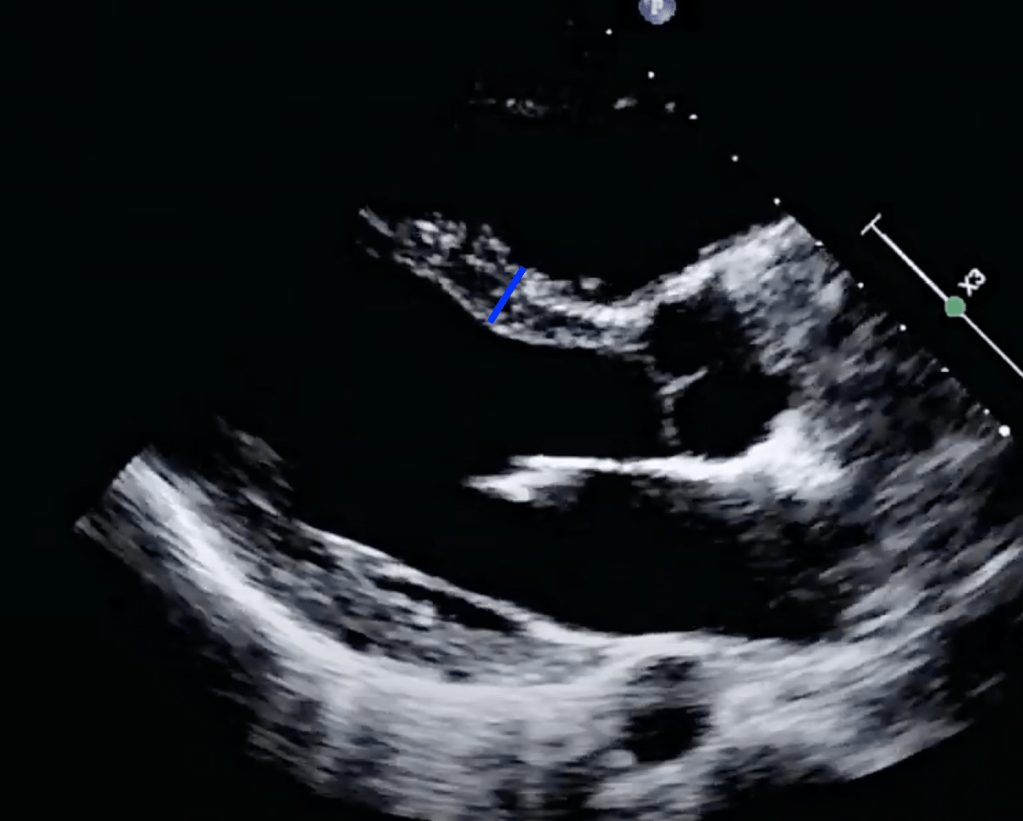
Looking at the initial EKG, you are concerned that this is possibly Wellens syndrome with Wellens waves in V2 and V3. While awaiting for cardiology to arrive, you obtain a bedside echo:
The bedside echo shows a reduced ejection fraction and looking through your records this is new when compared to his last echo.
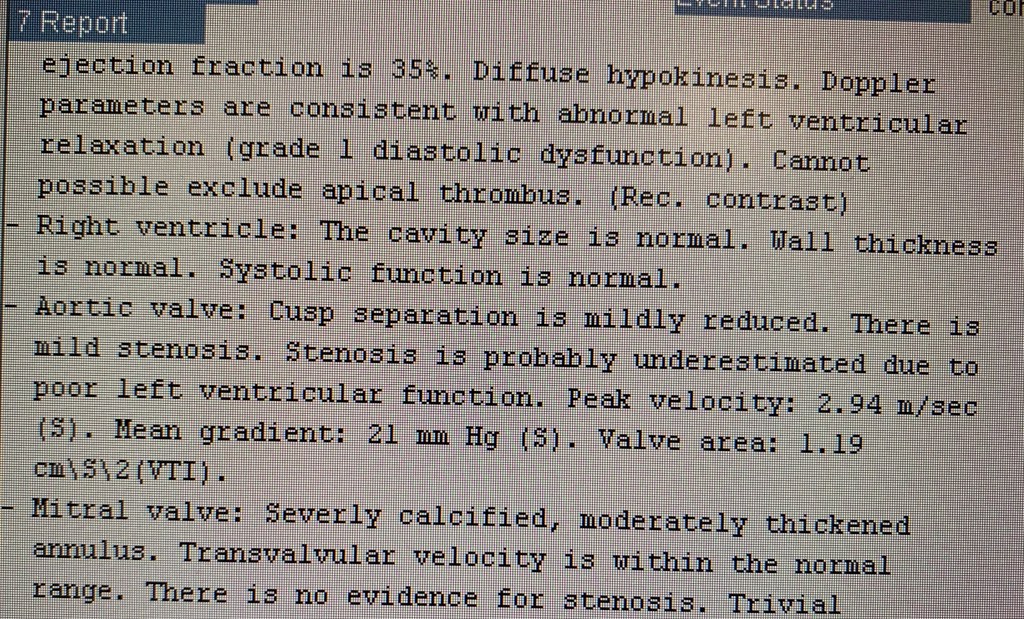
Ejection Fraction:
There are many different ways to measure ejection fraction with ultrasound (Simpson method, etc) that can be time consuming and require you to obtain multiple views. Furthermore, many of the methods require that your ultrasound have a cardiac package purchased and unlocked from the manufacturer in order to perform the measurements. Fortunately, an abundance of literature has come out that shows overall provider gestalt to be an accurate way to interpret the EF on bedside ultrasound when an exact measurement is not needed.
When obtaining a cardiac ultrasound, ask yourself if you feel the EF is hyperdynamic, normal, mildly reduced, moderately reduced, or severely reduced. There are three things you can look at while obtaining your images that will help you make this determination.
Mitral Valve Excursion
The mitral valve in a structurally normal heart should approach the septum during ventricular contraction. Below is a normal echo. Look how the mitral valve “slaps” the septum during each contraction. Go back to our image above and see that the mitral valve does not approach the septum during contraction.
https://gfycat.com/vapidfatherlygerenuk
Ventricular Cavity Size Reduction
With a normal EF, your ventricular cavity should moderately reduce in size during contraction. Imagine drawing a circle inside the area of the LV before contraction, and another one during contraction. The area of the circle should be smaller during contraction. If there is not much change, suspect a reduced EF.


Septal Wall Thickening
With an normal EF, the septum should moderate thicken during contraction. Imagine measuring the length of the septum that you have in view before contraction, and then again during contraction. The length should be longer during contraction. If there is not much change, suspect a reduced EF.

Summary
You will notice I did not give any exact measurements or size reductions for the three things discussed above. That is because all of these methods are subjective and again, have been shown in the literature to be an adequate estimation of EF when an exact measurement is not needed. These can quickly be utilized at the bedside and do not require any special features to be unlocked on the ultrasound machine. Quickly knowing if your patient’s EF is normal or reduced can greatly affect management.
Case Conclusion:
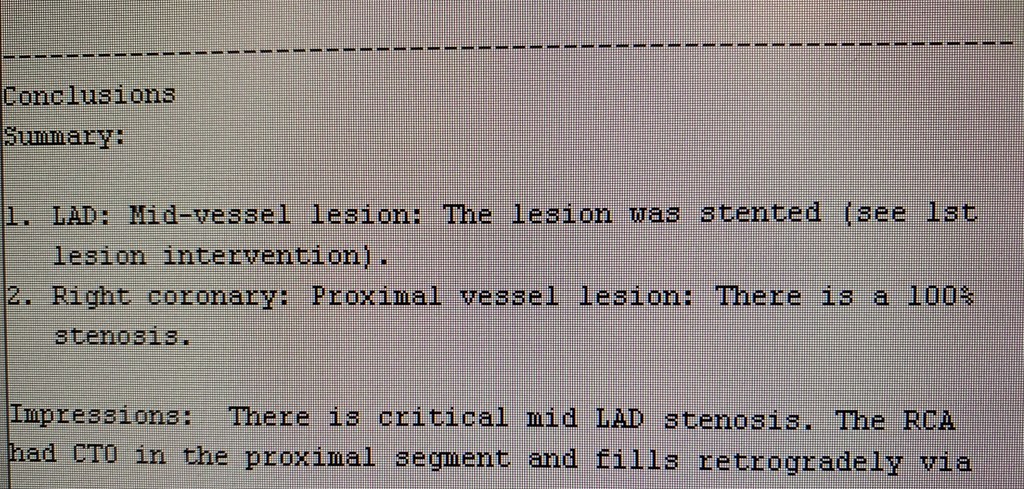
After completion of the ultrasound, cardiology arrives and the patient begins to have chest pain for the first time in the emergency department. A repeat EKG is obtained:
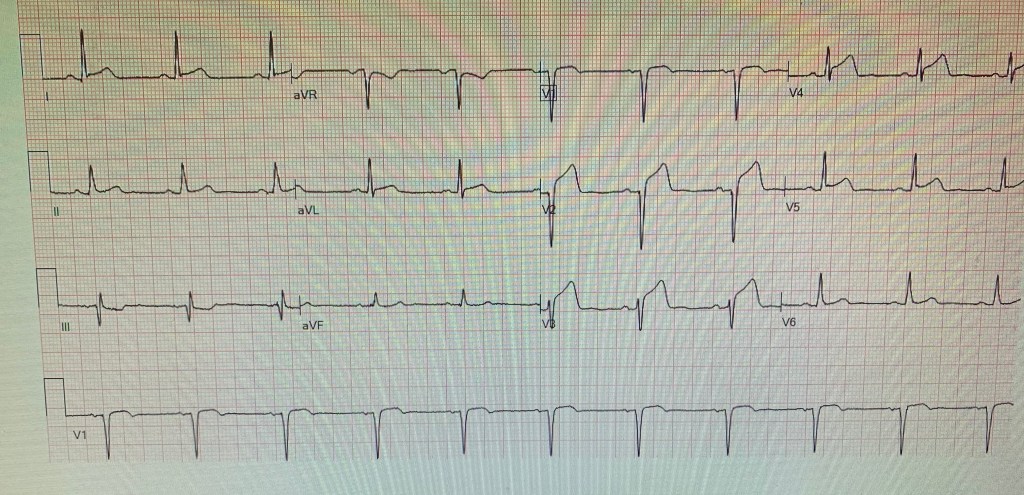
The patient goes to the cath lab and is found to have a critical LAD lesion, confirming your suspicion of Wellens syndrome.
Take Home Points:
- EF can be easily estimated at the bedside
- In most ER scenarios, an estimation of EF is sufficient for patient management
- Look at mitral valve excursion, LV area reduction, and septal thickening in order to make your estimate.
Author:
Timothy Beau Stokes, MD


You must be logged in to post a comment.