A 54 y.o male with a history of CAD and stents in the past presents for CP. Per pt, for the last two days he has been having mid sternal exertional cp radiating down his left arm, relieved by rest. Tonight the cp came on without exertion and has been persistent since. It does not radiate through to the back and it is not pleuritic. He has not noticed any leg pain or swelling. No infectious symptoms, vomiting, abdominal pain or shortness of breath.
The patient’s vital signs are BP 120/80. HR 65. 99% on RA and RR 18. On exam, the patient is diaphoretic. He has clear lungs, a benign abd, no JVD, no lower extremity edema or ttp, and no murmurs.
An EKG is obtained:

When compared to a prior EKG in our system, there are no changes.
Your high sensitivity troponin returns at 100. Your CXR is negative. The remainder of his blood work is unremarkable.
What can you do to help convince cardiology that this patient should go to the cath lab, even without a STEMI on the EKG and a trop of only 100?
You obtain a bedside echo:
The beside echo shows a mildly reduced EF as well as inferior and basal wall motion abnormalities. When compared to a prior echo in our system within the last year, these findings are new.
Wall Motion Abnormalities
Finding wall motion abnormalities with point of care ultrasound can be technically difficult, however when they are found they can be helpful and affect management. Providers need to be careful in distinguishing between acute and chronic abnormalities. Some patients after an ischemic event will chronically have wall motion abnormalities, and so seeing one on your ultrasound does not necessarily mean it is acute or a sign of ischemia. Without a prior echo to compare to, it is difficult to distinguish between the two.
The easiest way to find wall motion abnormalities is to save a video clip, and then scroll through it slowly on the machine while reviewing the clip rather than trying to see them in real time. Personally, I find visualizing wall motion abnormalities easiest on the parasternal short axis. Put your finger in the middle of the ventricle and then scroll through the clip image by image, watching the wall contract around your finger. Do all the walls contract symmetrically or does there seem to be one moving less and lagging behind?
Reviewing our patient’s echo, watch it again with the mouse pointer in the middle of the ventricle of the PSSA clip (imagine your finger being where the pointer is):
There is an area of the wall that is moving less than the other areas (remember this would be easier to see if you slowed down the clip/scrolled through the clip image by image on the machine itself):
You can also see this on the PSLA, although it is more subtle:
Case Conclusion:
After your bedside echo, you contact cardiology who reviews your images and orders a stat cardiology based echo. The report shows:

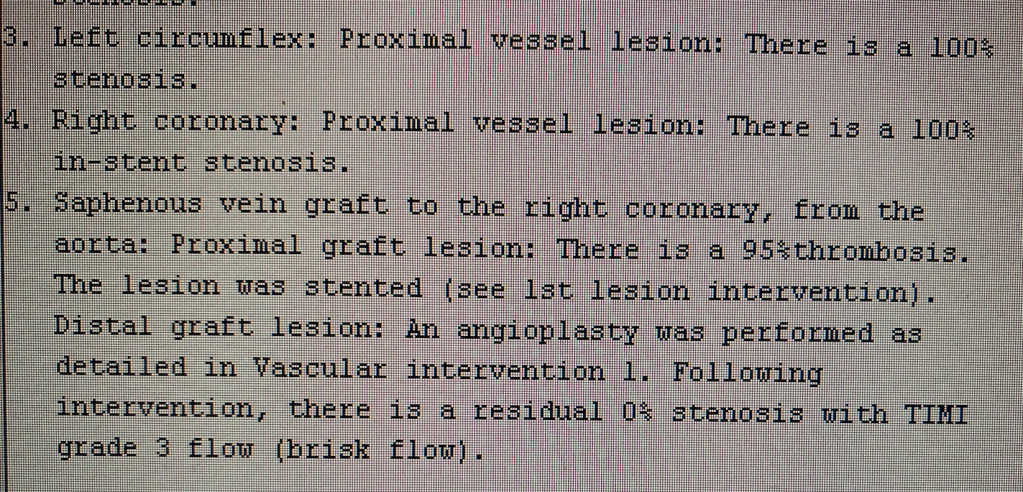
Based on his concerning history and these echo findings, even with a normal EKG cardiology decides to take the patient emergently to the cath lab. His cath shows:
The patient did well post cath and was discharged home after a short hospitalization.
Take home points
- Regional wall motion abnormalities can be technically difficult to obtain and visualize, but when found can be helpful.
- Differentiate between acute and chronic abnormalities – some patients will chronically have wall motion abnormalities.
- Save your video clip and then play it back slowly, frame by frame, to find the wall motion abnormality.
- Remember that some patients need emergent catheterization, even without a STEMI on the EKG.
- Remember that troponin can be unimpressive early on in ischemia. Our patient’s trop ended up peaking at 70,000 even though the first one was 100.
Author:
Timothy Beau Stokes, MD


You must be logged in to post a comment.