A 70 y.o female with T2DM, HTN, CKD, CHF, Hypothyroidism presents via ambulance from home for AMS. Report via EMS is the patient was febrile at home yesterday, and family called EMS this morning due to patient speaking to people in the corner of the room that were not actually there. The patient was found to be bradycardic to 53 in the field.
On arrival to the ER, the patient is confused with GCS 13 (M6, V4, E3), AOx1 to name only. Her face is severely swollen with bilateral periorbital swelling and a mildly swollen tongue. Her heart rate is bradycardic at 55, and EKG shows AV dual paced rhythm. Her temp is concerning for hypothermia to 31C. Bair hugger was placed and warmed fluids were started.
PMH:
- Type 2 DM
- HTN
- CKD
- CHF
- Hypothyroidism
Surgical Hx:
- Hernia unknown type or date
- Bilateral knee replacements 1994 & 2004
- Pacemaker Boston Scientific placed 5/28/2015
- Ovarian cyst removal
Social Hx:
- No noted tobacco, alcohol, or drug use
Vital Signs:
- BP 136/51, P 55, R 16, O2 Sat 96% RA, T 31.2
Physical Exam:
Constitutional: GCS 13 (M6, V4, E3). AOx 1 to name only. Cool and dry to touch. Mumbling to herself.
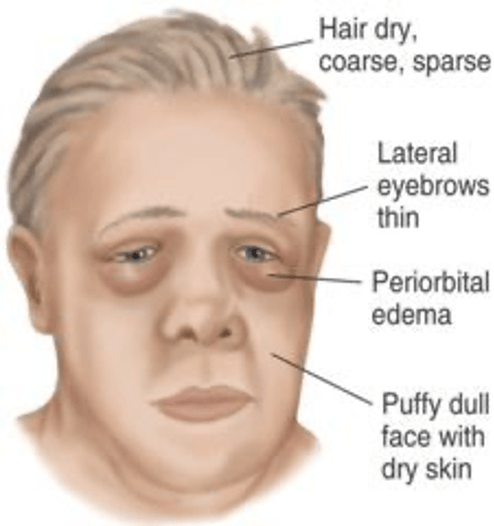
HEENT: Normocephalic. Atraumatic. Periorbital swelling and puffy face. Bilateral corneal opacity, right eye minimal reactive to light. Ears clear. Oropharynx significant for mild tongue edema. Mucous membranes tacky and pale. Trachea midline.
Cardiopulmonary: Bradycardia, regular. No MRG. No JVD. Diminished lung sounds at the bases, otherwise clear. Equal and full pulses bilateral radial and DP.
Abdomen: Obese, NT, BS+. No peritoneal signs. Diffuse irritant dermatitis of intertriginous areas.
Extremities: Upper extremities unremarkable. Bilateral lower extremities significant edema with irritant dermatitis throughout as well.
Skin: Diffuse intertriginous irritant dermatitis with bilateral lower extremities weeping fluid and excoriation sites moist and raw.
Neuro: Confused with GCS 13, AO x 1 to name only. No focal neuro deficits appreciated. Altered so unable to get full neuro exam. DTRs normal bilateral patellar tendons. No clonus or asterixis.
Labs and Studies:
- Initial: CBC, CMP, UA, BC x 2, Lactic Acid, EKG, troponin, CXR, CT head
- Follow up: CT abd/pelvis, TSH, Free T4, Serum cortisol
ED Course:
- 2 L normal saline (warmed with ranger) & Bair hugger, nystatin powder, Zosyn 3.375 g IV and Vancomycin 1 g IV
After the above interventions, labs began to return and were not consistent with sepsis. The patient did not have an adequate response to the above interventions and so the differential and plan was reconsidered. The patient was still hypothermic, bradycardic, and began to become hypotensive with SBP in the low 100s.
The TSH came back mildly elevated at 8.8, free T4 low normal 0.85, and serum cortisol normal at 13.3. Although these labs were only mildly abnormal, her clinical picture was concerning for myxedema coma and so endocrinology was consulted. They agreed and recommended levothyroxine and hydrocortisone. The patient was admitted to the ICU.
Myxedema Coma
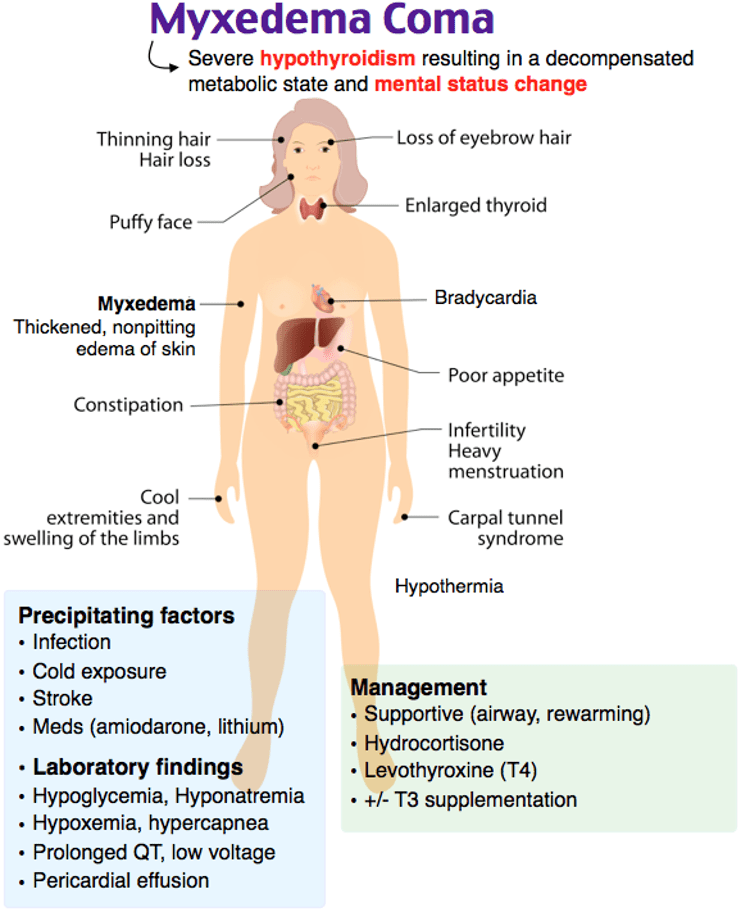
Myxedema coma is a disease state consisting of severe hypothyroidism leading to varied combinations of altered level of consciousness, bradycardia, hypotension, hyponatremia, hypoglycemia, hypoventilation, and hypothermia. The hallmarks of the diagnosis are AMS and hypothermia, with varying degrees of the other findings.
Despite the name of myxedema coma, many presentations lack coma on presentation and have some form of altered mental state from lethargy to obtundation to psychosis (termed “myxedema madness”). It has also been reported that seizures have occurred as a type of neurologic sequelae.
Approximately 50% of patients will have hyponatremia which can be associated with the above neurologic findings. Even further, measuring a cortisol level in these patients is a good idea as some have also been noted to have adrenal insufficiency.
The majority of patients will have hypothermia and AMS as stated above. The degree of hypothermia has been noted as a strong indicator of prognosis, as the lower the temperature the more likely the patient will succumb to the illness.
Hypoglycemia can also be found in this disease state as thyroid hormone and adrenal regulation play important roles in euglycemia in the healthy individual. In these patients, they will have a combination of low thyroid and occasionally adrenal insufficiency, both contributing to poor gluconeogenesis.
Cardiovascular abnormalities such as hypotension and bradycardia have long been taught in the medical textbooks as a hallmark of this disease, but myocardial suppression is a rarer finding that previously thought. Although patients can develop CHF from severe hypothyroidism, many of the patients that actually present with hypotension or pulmonary edema are patients that already have a hx of CHF prior to their severe hypothyroidism. If patients develop CHF from the hypothyroidism it should be reversible with thyroid replacement therapy.
Physical exam findings consistent with myxedema coma include edema of the hands and face including the nose, tongue, and lips secondary to albumin and mucin deposition in the skin and other tissues.

Diagnosis:
TSH, Free T4, Serum Cortisol
Laboratory values consistent with myxedema coma are elevated TSH, low Free T4, and low serum Cortisol. Usually the first test to obtain would be a TSH and this should be elevated in severe hypothyroidism. The free T4 level should be very low, however, in rare cases it may be less severely decreased or even low normal. If the clinical history and physical exam findings fit, be sure to discuss with endocrinology.
Considering the common concomitant primary adrenal insufficiency present in some of these patients, serum cortisol levels can also be measured. These values however can be less reliable in the emergency department as they vary throughout the day and ideally should be measured in the AM before and after cosyntropin administration.
There has been a proposed scoring system for patients with myxedema coma:

Of note, this particular patient scored 60 for Thermoregulatory Dysfunction < 32, Somnolent/lethargic, present precipitating event, Bradycardia 50-59, and Decrease in GFR.
Treatment:
- Thyroid Hormone
- Combination of T3 & T4 administration suggested
- Levothyroxine 200-400 mcg IV bolus followed by 50-100 mcg daily
- Liothyronine 5-20 mcg IV bolus followed by 2.5-10 mcg q8hours
- Glucocorticoids
- Hydrocortisone 100 mg IV q8hours
- Supportive Measures
- Appropriate measures of coexisting problems (eg, infection)
Take Home Points:
- Remember the hallmarks for Myxedema Coma are AMS and Hypothermia with varying degrees of hypotension, bradycardia, hypoglycemia, hyponatremia, and hypoventilation.
- Do not eliminate this from your differential if you have a low normal T4 level. If the clinical history fits, consult endocrinology.
- Treatment consists of combination T3, T4 and glucocorticoids
Authors:
William Hall IV, MD
Peer Reviewed and Edited By:
Dylan Kellogg, MD
Timothy Stokes, MD


You must be logged in to post a comment.