A 24 y.o m presents with several months of swelling over the elbow area. The patient noticed non painful swelling over the inner aspect of his elbow several months ago, but he never saw a physician. The swelling has not increased, however over the last two days it has become painful. He has not noticed any overlying skin changes or pain anywhere else in the arm. No other symptoms. No significant past medical history.
On exam, his vitals were normal. He had a palpable mass medial to the olecranon which was tender to palpation. It was not fluctuant. No overlying skin changes. No crepitus. No joint effusion. ROM intact of the entire extremity and the limb was neurovascularly intact.
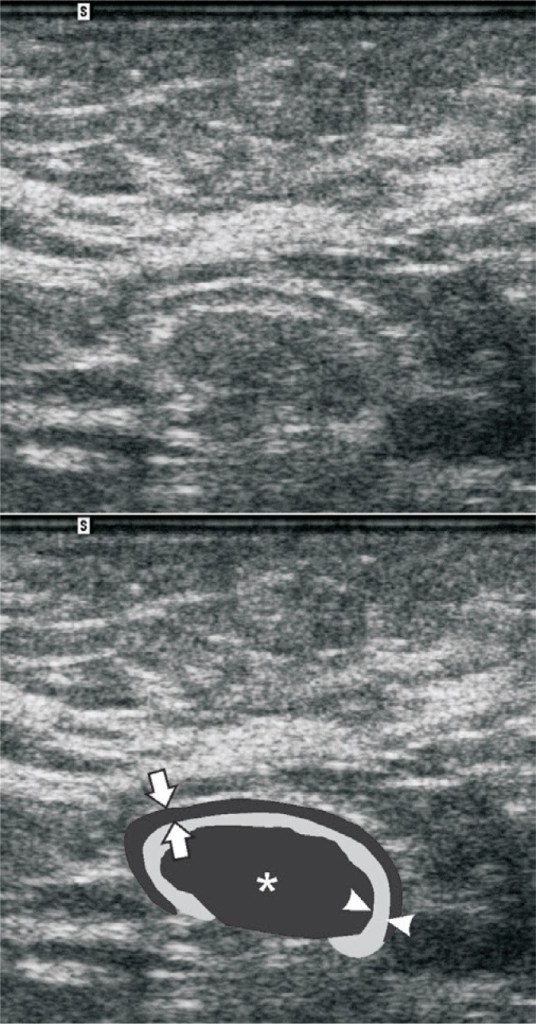
A bedside US was obtained of the area which showed:
Ultrasonography of Lymph Nodes:
Ultrasonography of lymphadenopathy can be technically difficult. Differentiating benign lymphadenopathy from malignant lymphadenopathy can be even harder. Given this, many would argue that routine point of care ultrasonography of lymphadenopathy for medical decision making should be deferred for a radiology based study. However, emergency providers should still be familiar with both typical and atypical appearances of lymph nodes on ultrasound as their appearance can cause misidentification of both the lymph nodes themselves and other surrounding structures.
Typical Lymph Node Appearance:
A typical lymph node should appear as a hypoechoic structure with an echogenic hilum:
Malignant Lymph Node Appearance:
Some characteristics of malignant lymph nodes are eccentric hypertrophy, lack of an echogenic hilum, large size, cystic or necrotic areas, ill defined margins, and heterogenous appearance:


Pitfalls:
Normal lymph nodes, benign lymphadenopathy, and malignant lymphadenopathy all can mimic other structures on ultrasonography which is why the emergency physician should be aware of their appearance. Be aware of the anatomical distribution and location of lymph nodes to avoid misclassifying a lymph node as a blood vessel. Also obtain images in both longitudinal and transverse positions. Blood vessels will look very different in longitudinal and transverse positions however lymph nodes will retain their round appearance. If there is something that appears to be a fluid collection, search the surrounding area for other “fluid collections” as lymph nodes tend to appear in chains. Be aware that some fluid collections may contain separations and heterogenous material and can mimic lymph nodes. If in doubt, obtain a radiology based study.
Lymph node mimicking fluid collection:

Lymph node mimicking clot:

Case Conclusion:
The ultrasound obtained in our patient showed epitrochlear lymphadenopathy. A radiology based study was obtained and was interpreted by radiology as unable to rule out malignancy and they recommended a future lymph node biopsy.

Palpable epitrochlear lymphadenopathy is always pathological. The differential includes extremity infections, lymphoma, sarcoidosis, tularemia, and secondary syphilis. The patient had a primary care appointment secured for him to continue the work up of his lymphadenopathy but was unfortunately lost to follow-up.
Take Home Points:
- Differentiation between benign and malignant lymphadenopathy can be technically challenging. Consider obtaining a radiology based study.
- Beware that both normal and abnormal lymph nodes can mimic other structures and pathologies on ultrasound, including fluid collections and DVTs.
- Obtain images in both transverse and longitudinal axises to aid in identifying the structure – for instance a lymph node may appear similar in both axises but a vessel will not.
- If in doubt, obtain a radiology based study.
Author:
Timothy Beau Stokes, MD

You must be logged in to post a comment.