A 3 year old male presents to the emergency room with a fever. His parents state that the fever has been present for 5 days and is associated with rash, lymphadenopathy, erythema of the lips, and “pink eye.”
A case presentation such as this one is obviously pointing towards Kawasaki disease, however many cases presenting to the emergency room are not as clear cut. Kawasaki disease is a vasculitis that affects children and causes prolonged fever as well as several inflammatory signs. The reason this is a can’t miss diagnosis is due to the cardiac complications including coronary artery aneurysms, heart failure, myocardial infarction, arrhythmias and decreased cardiac function.

Kawasaki Disease
The cause of Kawasaki disease remains unknown but is thought to be related to an autoimmune response which leads to inflammation of arteries and mucocutaneous tissue. Patients will seemingly have a self limited viral URI or GI illness associated with persistent fevers. These persistent fevers lasting 5 or more days will then be associated with oral mucous membrane changes and extremity rashes. Other common symptoms include bilateral ocular conjunctivitis and cervical lymphadenopathy.
The disease itself is self limiting lasting about 12 days. The reason this disease should stay at the forefront of every EM physician’s mind is the coronary artery abnormalities. Cardiac complications in Kawasaki include dilation, aneurysm and stenosis with reported cases of pericardial effusions, peripheral artery aneurysms and valve regurgitation.
Aneurysms have a 50% chance of returning to normal 4-6 weeks later. As a result of the systemic inflammation, vessels will be infiltrated by neutrophils/lymphocytes/macrophages leading to changes in the elastic lamina of the vessel. This inflammation leads to changes in epi/peri/endocardium and AV nodes. As a result, these patients can present with tachycardia far higher than expected with fever, a hyperdynamic precordium, murmurs or gallops.
Diagnosis

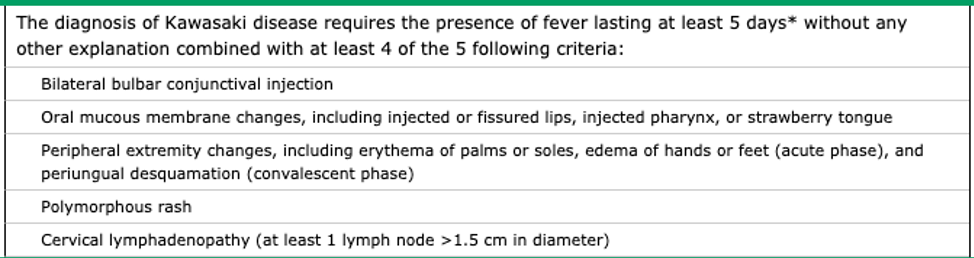
Along with a fever of over five days, a diagnosis requires at least four of the following criteria as well:
Bilateral conjunctival injection
Bilateral non exudative conjunctivitis will be present a few days after fever with most cases alongside photophobia. Anterior uveitis has been seen in 70% of cases.
Polymorphous rash
Seen as erythema or desquamation with macular skin lesions on the trunk/extremities.
Mucositis
The patient’s mouth will have cracked red lips with an inflamed tongue and sloughing. Has been described as “strawberry tongue.”
Peripheral extremity changes
Patients will often have erythema/edema on their extremities with possibility of periungual desquamation developing as well.
Cervical lymphadenopathy
Anterior cervical lymphadenopathy will be present in 25-50% of cases.
Other (not counted towards diagnostic criteria):
Symptoms often seen during the prodrome phase are diarrhea/vomiting, irritability, cough.
Incomplete Kawasaki Disease
Simply following the criteria for Kawasaki disease led to a subset of undiagnosed children having coronary artery abnormalities. As a result, guidelines for incomplete (atypical) Kawasaki were made and include patients with >5 days of fever with 2-3 clinical criteria, or patients less than six months of age with unexplained fever for >7 days even with no other criteria. Laboratory markers and UA changes can be used to help support the diagnosis of incomplete Kawasaki disease.

Labs/Imaging
Kawasaki Disease is a clinical diagnosis that may be supported by inflammatory markers such as CRP and ESR. Urine microscopy was shown to indicate elevated WBCs. Half of patients have elevation in transaminases.
Echocardiogram must be ordered to establish baseline heart function, especially in scenarios of delayed disease presentation.
Treatment:
The mainstay of treatment for patients with Kawasaki is intravenous immune globulin (IVIG) and aspirin. Studies have shown that treating with IVIG within the first 10 days of disease will lead to a decrease of coronary artery aneurysms from 25% to less than 5%. The IVIG dose is 2 g/kg ran over 8-12 hours with an aspirin dose of 30-50 mg/kg per day divided into four doses until fever has subsided for 48 hours. Once fever has stopped for 48 hours, aspirin may be switched to a low dose of 3-5 mg/kg/day.
As a result of early diagnosis and treatment with IVIG/aspirin, mortality of Kawasaki has decreased and is currently 0.1%. Nevertheless, these patients should be admitted to pediatrics with an infectious disease consult.
Take Home Points:
- Diagnosis of Kawasaki Disease is clinical and includes >5 days of fever with 4 out of 5 supporting criteria/symptoms.
- Incomplete Kawasaki must also be considered in patients with fever >5 days with 2-3 clinical criteria or patients younger than 6 months with seven days of fever. Obtain labs/inflammatory markers/UA to help support the diagnosis.
- The feared complication of this disease is coronary artery aneurysm. Suspected Kawasaki disease gets admitted for treatment with IVIG and ASA (usually determined by infectious disease).
- Obtain a baseline echocardiogram.
Authors:
Hakkam Zaghmout, MD
Peer Reviewed and Edited By:
Timothy Stokes, MD


You must be logged in to post a comment.