A 75 y.o m with a PMH of long term smoking presents for abdominal pain. On arrival, the patient is hypertensive and has a pulsatile mass on abdominal exam. He has no known medical issues as he does not like to see doctors and has not seen one in over 10 years. Besides the pulsatile mass, the patient is well appearing and his abdominal exam is otherwise benign.
You obtain a bedside ultrasound:
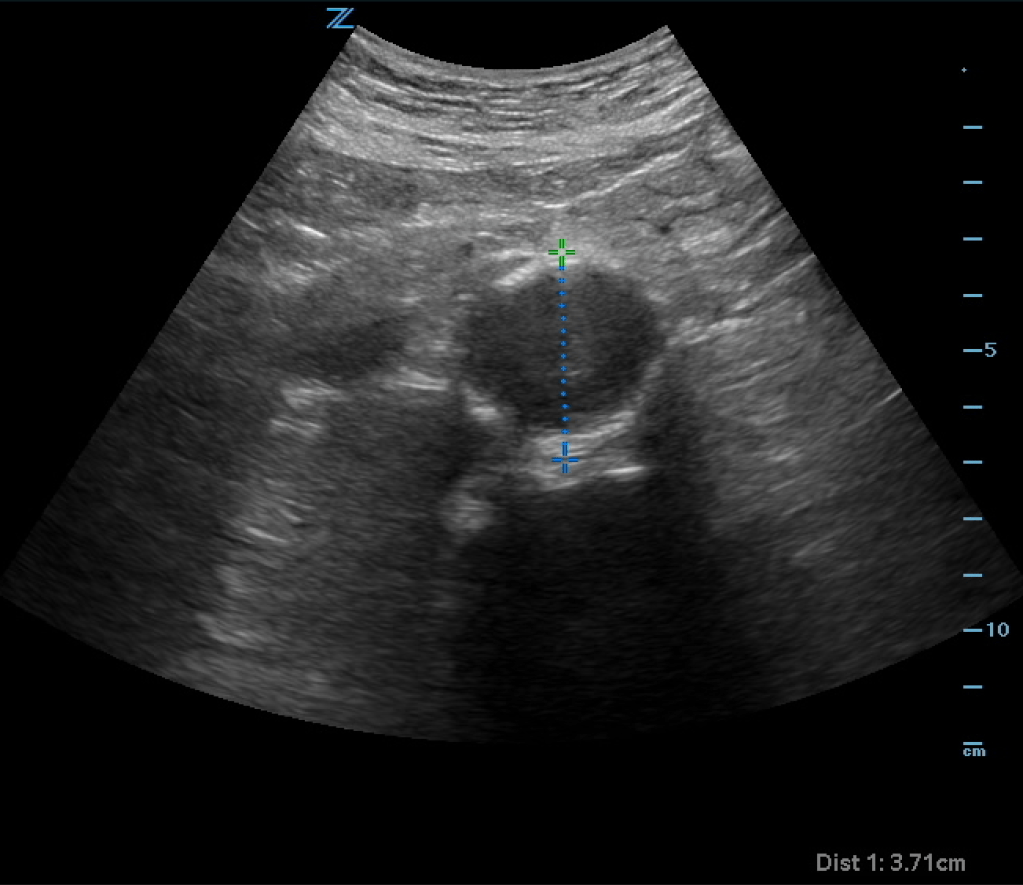
The ultrasound shows an enlarged aorta concerning for AAA, measuring at 3.71cm. However looking closely at the aorta, it almost appears as if there is a dissection flap with potentially two lumens on the ultrasound. You obtain color doppler:
Color shows there are two areas in the aorta, one with flow and one with no flow concerning for potential dissection vs thrombus. CTA of the abdomen and pelvis is obtained and shows:
CT shows a AAA without rupture. There is an area of thrombus seen on the CT which correlates with the ultrasound findings seen above. There is no true dissection flap.
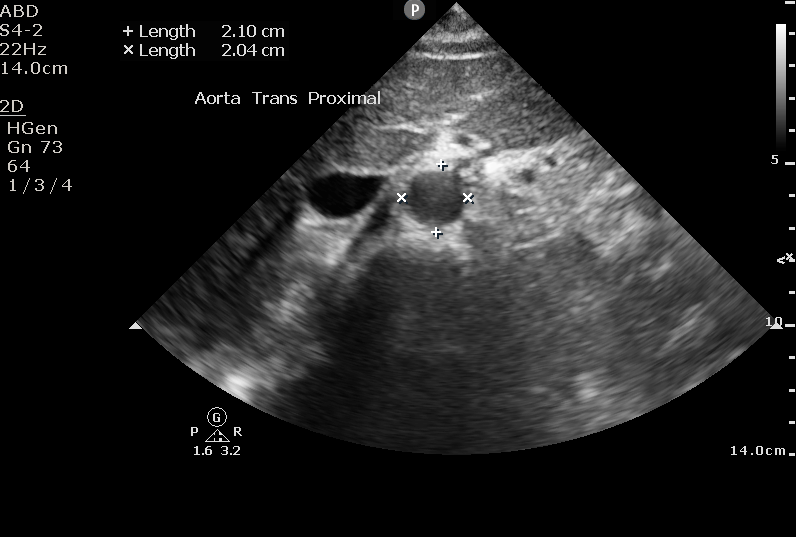
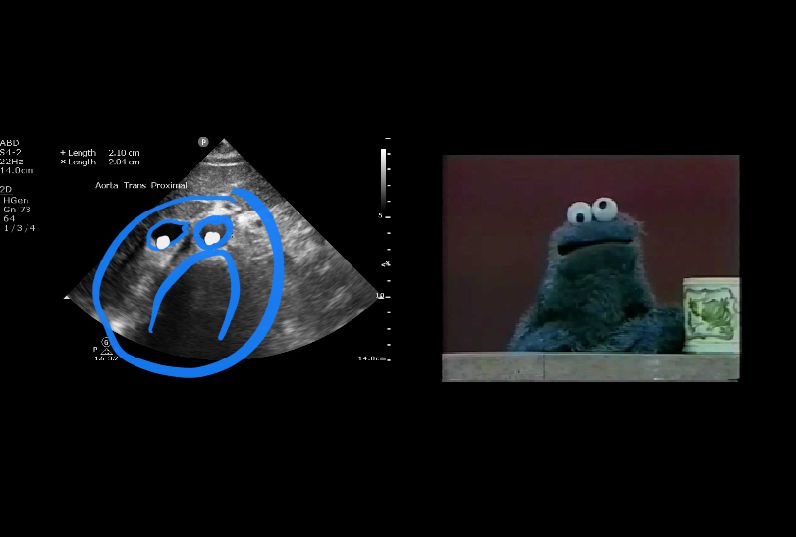
Aortic Ultrasound
Identify the aorta based on anatomy, not on pulsatility or color flow (there are times where the IVC can appear to be pulsatile and may lead to misidentification). The aorta should appear as a “sad cookie monster” with the IVC and aorta making up the eyes, and the vertebral body making up the frown. You can identify the vertebral body as a hyperechoic “frown” with anechoic shadow behind it.
You should attempt to locate the major branches when ultrasounding to aid in proper identification and to ensure you are scanning the entire aorta. Obtain views of the celiac, SMA, and aortic bifurcation.
The celiac can be identified from the “seagull sign.” The celiac, hepatic artery, and splenic artery form a seagull shape.


The SMA can be identified from the “matador sign.” The SMA, PV, and SV form a matador hat like shape.
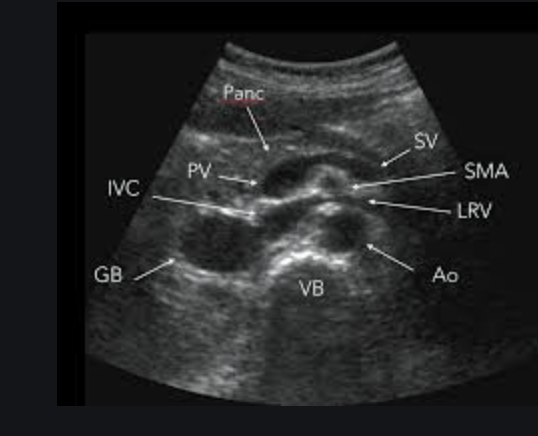

Measure the aorta anterior the posterior, outside wall to outside wall. We want to overestimate the size in order to be as sensitive as possible. Fusiform aneurysms that would only show up with lateral wall to lateral wall measurements are very rare. Also, the lateral walls on ultrasound will be less accurate due to the direction of the beam and artifact than the anterior and posterior walls. Normal aortic measurement should be less than 3cm, with the risk of rupture greatly increasing over 5.5cm.
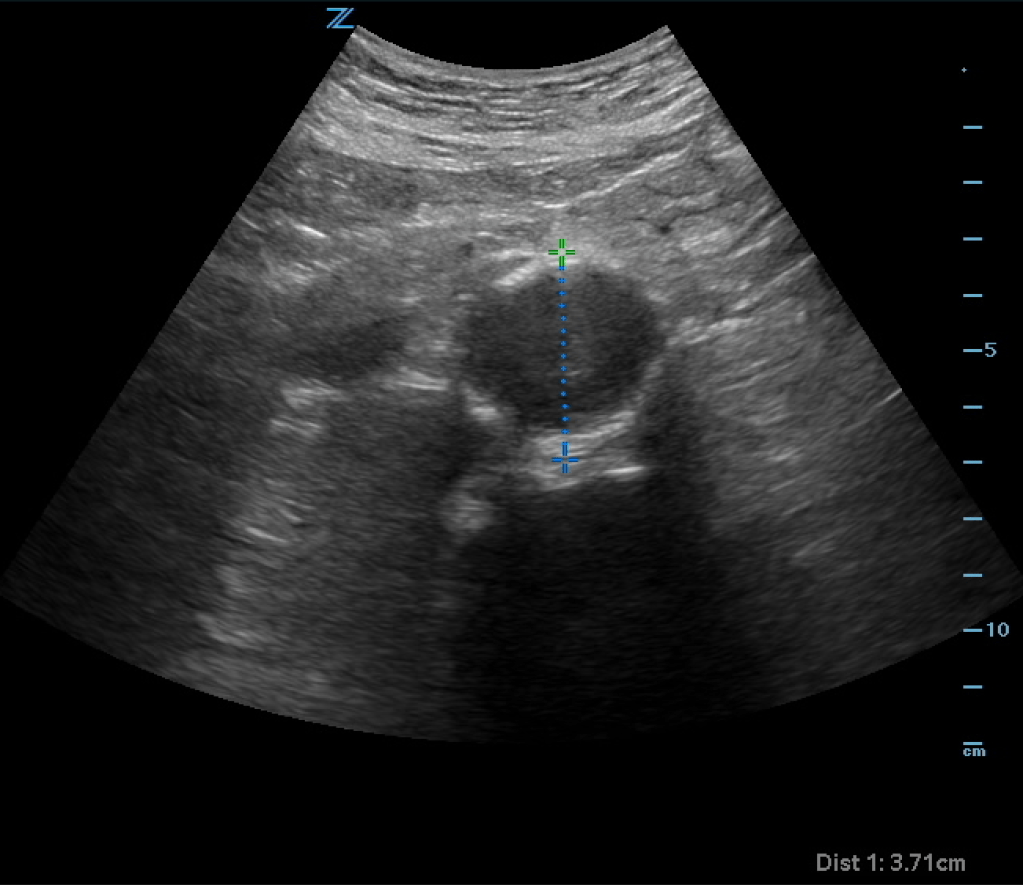
Remember that the aorta is retroperitoneal. Many times you will not actually see free fluid or evidence of rupture on ultrasound. A AAA on ultrasound plus abdominal pain is a ruptured AAA until proven otherwise. If you are concerned about dissection, you may see the flap and false lumen (color doppler may aid in the diagnosis) on ultrasound, but an ultrasound is not sensitive enough to rule out dissection. Obtain a CTA to evaluate the aorta. Also remember that thrombus is common in AAA and actually helps stabilize the aneurysm. In a normal caliper aorta however, thrombus should be considered evidence of underlying dissection (even if a dissection flap is not seen) until proven otherwise.
Case Resolution:
CTA of the abdomen/pelvis confirmed a 3.71cm AAA without rupture or dissection. Thrombus was visualized on the CT which explained the ultrasound findings. Vascular surgery evaluated the patient and recommended serial outpatient ultrasounds and cleared the patient for discharge.
Take home points:
- Use anatomy to identify the aorta on ultrasound
- Measure the aorta anterior to posterior, outside wall to outside wall to get the most sensitive measurement
- A normal aorta diameter is < 3cm
- Abdominal pain plus AAA on ultrasound is ruptured AAA until proven otherwise
- Although in a normal caliper aorta thrombus on CT can be a sign of underlying dissection, thrombus is common in a AAA and actually helps stabilize the aneurysm
Author:
Timothy Beau Stokes, MD

You must be logged in to post a comment.