A 34 year old male with a medical history of hypertension, hyperlipidemia and chronic liver injury secondary to alcohol abuse presented to the emergency department with diffuse abdominal pain and more than 30 episodes of vomiting over the past 12 hours. The patient admitted to increased alcohol intake over the past two days, however stated he started getting abdominal pain and vomiting and so began to not be able to drink his usual amount of alcohol.
Patient appeared uncomfortable on exam. He was afebrile but was tachycardic to the 130’s. His abdominal exam revealed right upper quadrant tenderness to palpation. Differential initially included hepatitis, biliary pathology, pancreatitis, bowel obstruction and alcohol withdrawal for which initial management included CBC/CMP, lipase and a RUQ ultrasound.
Ultrasound was negative for biliary pathology. Labs were significant for hypokalemia, leukocytosis, mild hepatitis, and an anion gap of 20. Further workup was obtained.
Alcoholic Ketoacidosis
Alcoholic ketoacidosis is typically seen in patients with chronic alcoholism but can also occur in otherwise healthy patients after episodes of excessive binge drinking. Patients who are malnourished, secondary to chronic alcoholism, have particularly severe presentations for which symptoms include abdominal pain, nausea and emesis. As symptoms increase in severity, patient’s often stop drinking alcohol and by the time they present to the emergency department, blood alcohol level may be low or even undetectable.

Pathophysiology
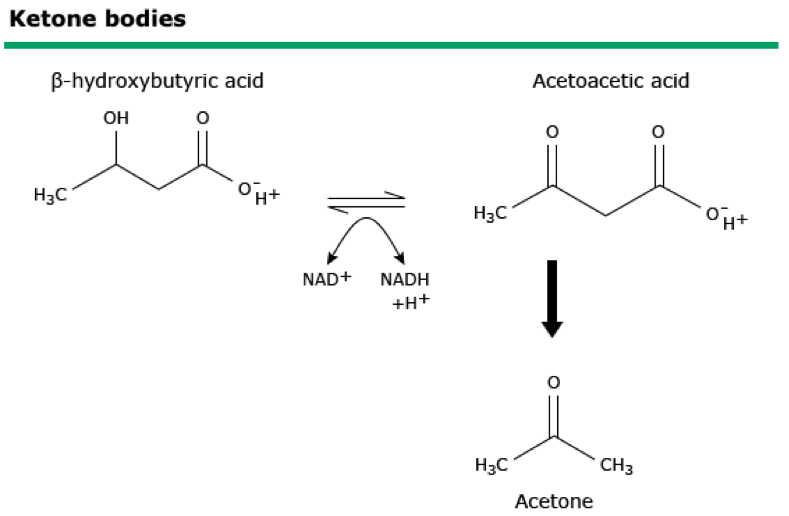
In the event of low glucose, the body begins to rely on ketones. Ketones are compounds derived from the metabolism of fat, and are: acetone, acetoacetic acid and beta hydroxybutyric.
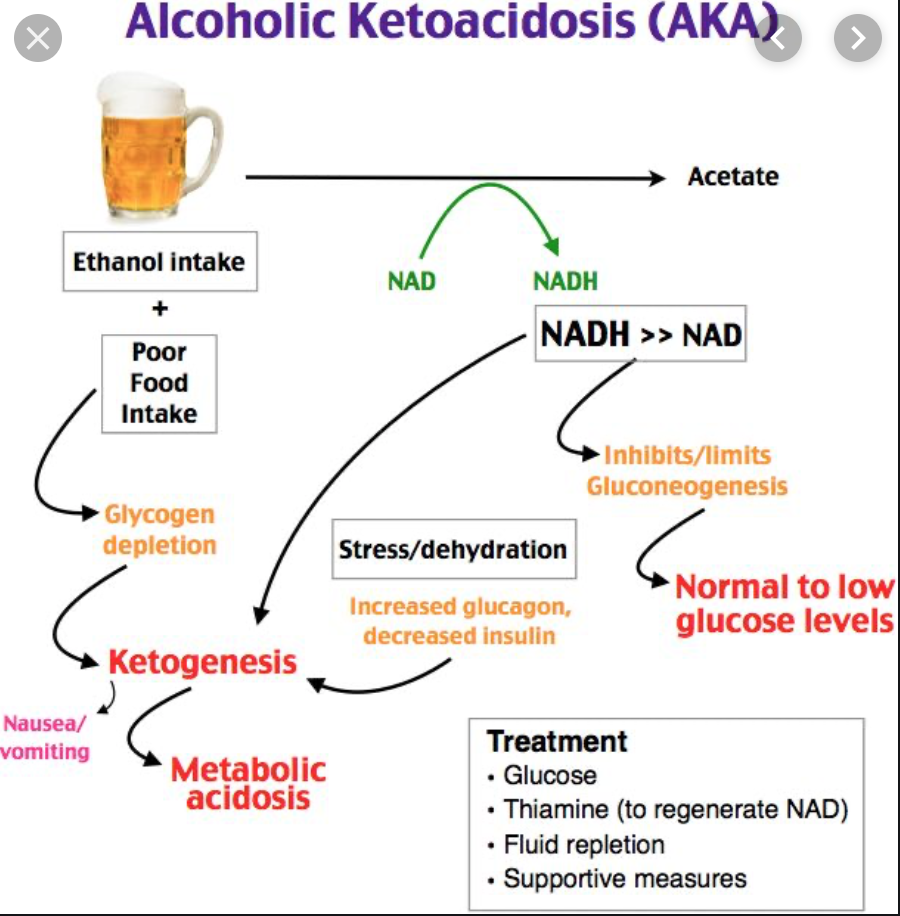
The creation of ketone bodies by the liver is in the presence of low insulin levels/high glucagon levels, and long chain fatty acids available in the hepatic mitochondria. In this scenario however, ethanol is oxidized by the liver into acetaldehyde and then acetic acid. This is then converted to acetyl-CoA and can then be used in one of three pathways:
- Krebs cycle
- Fatty acid synthesis
- Ketogenesis and the formation of acetoacetic acid, acetone or beta hydroxybutyric acid
In the presence of excess acetyl Co-A, the kreb cycle becomes saturated and acetyl-CoA enters the ketogenic pathway to create ketone bodies.

With binge drinking or withdrawal from alcohol, ethanol level decreases resulting in catecholamine/cortisol levels to rise leading to a hormonal response of fasting (the previously discussed low insulin/high glucagon) thus leading to lipolysis and fatty acid oxidation. Ethanol is then oxidized to acetaldehyde and then to acetic acid. This reaction leads to three clinically relevant factors:
- Suppression of gluconeogenesis and possible hypoglycemia
- Acetoacetic acid/beta-hydroxybutyric acid ratio begins to favor beta-hydroxybutyric acid which does not affect clinical presentation but is useful in diagnosis.
- Conversion of pyruvate to lactate becomes favored leading to hypovolemia, heart failure and sepsis.
Clinical Presentation
Patients with alcoholic ketoacidosis will present with nausea, vomiting and abdominal pain following alcohol withdrawal or an episode of binge drinking. Hypovolemia, tachycardia and the following electrolyte abnormalities are often seen:
Hypo/hyperglycemia
Glucose measurements may slightly vary. Patients may present with either hypo- or hyper-glcyemia. However, as opposed to diabetic ketoacidosis (DKA) where glucose is typically exceedingly high, in alcoholic ketoacidosis, glucose tends to be less than 275 mg/dL.
Hypokalemia
Diabetic ketoacidosis (DKA) classically presents with falsely elevated potassium levels primarily due to hyperosmolality secondary to hyperglycemia and insulin deficiency causing an increase in potassium redistribution into extracellular space.
This is unlike alcoholic ketoacidosis in which the acidosis will cause a hydrogen ion buffer that maintains an electroneutrality, thus preventing potassium from shifting out of the cell. Thus, in most cases a patient will have a lower measured initial potassium than expected.
Hypomagnesemia
This is in fact much more common in patients with alcoholic ketoacidosis than DKA. Potentially due to dietary deficiency, urinary magnesium wasting, diarrhea or pancreatitis.
Hypophosphatemia
Due to decreased intestinal absorption and increased excretion, hypophosphatemia may occur. However, initially due to metabolic acidosis and insulin deficiency, phosphate is pushed out of the cell.
Anion gap
Diagnosis of ketoacidosis is made by elevated anion gap with presence of ketone bodies. A ketoacidosis with normal glucose is diagnostic of fasting/alcoholic ketoacidosis with the difference in diagnosis made by presenting history.

Diagnosis
In the past, diagnosis was made with urine dipstick and nitroprusside tablets. Ketone testing would be done with the limitation of not knowing the extent of acidosis or anion gap. These limitations have led to the direct measurements of beta hydroxybutyrate, one of the by products of ketogenesis discussed previously.
Differential diagnosis in a patient presenting with an alcohol abuse history must also include fasting ketoacidosis, lactic acidosis, high anion gap metabolic acidosis, methanol/ethylene glycol poisoning with consideration for uremic acidosis. Along with CBC, CMP, lactic acid, and beta hydroxybutyrate level, the following tests should also be ordered:
- Urine/serum ketone bodies
- Creatinine to detect kidney disease
- Salicylates to rule out excessive use/overdose
- Serum osmolality
Commonly there will be a combined acid base disorder as result of the ketoacidosis alongside hyperventilation or in our patient’s case, vomiting. As seen by our VBG, patient had an alkalotic pH, with ketoacidosis at presentation.
Treatment
Initial management should include 100 mg of thiamine provided IV/IM, prior to any glucose containing solutions in order to avoid Wernicke’s encephalopathy.
Alcoholic ketoacidosis should be treated the same as fasting ketoacidosis with dextrose/saline solutions. Dextrose will increase insulin, reduce glucagon and slow down the process of ketogenesis. These should be done even in patients with normal glucose levels. In patients with high glucose levels, consider insulin infusion possibly in combination with a dextrose infusion to reverse ketone body formation.
In severe hypokalemia, consider delaying the dextrose infusion until potassium is aggressively replaced as the dextrose infusion will cause release of insulin and further reduce potassium levels.
Normal saline/isotonic fluids need to be aggressively used to resolve hypovolemia which further contributes to ketogenesis. Hypovolemia and renal electrolyte loss promote glucagon secretion and ketone body formation.
Case Resolution
Our patient had a mixed acid/base disorder. When it was found that he had an elevated anion gap, the workup was expanded to attempt to find the contributors of the anion gap. Tylenol, aspirin, and toxic alcohols were negative. Lactic acid was not elevated enough to explain the magnitude of his gap. He was not uremic. Ketones were positive both in the urine and with an elevated beta hydroxybuterate.
Our patient had been having severe, frequent vomiting. This had caused profound hypokalemia and an alkalosis that masked his anion gap metabolic acidosis secondary to ketone bodies. The patient was given aggressive IV hydration and potassium supplementation and then an infusion of dextrose containing fluid was initiated on admission. His acid base disorder resolved as well as his ketones, and his anion gap closed.
Take Away Points
- Alcoholic ketoacidosis presents as an acute acidosis secondary to ketone bodies and can be found in both daily alcohol users as well as binge drinkers
- Initial treatment should include dextrose containing fluid, even if the patient is not hypoglycemic. The goal is to shift metabolism away from generating ketone bodies.
- Patients will need aggressive saline hydration to replace losses from vomiting and polyuria which further contribute to the ketosis.
- Aggressively treat hypokalemia, hypomagnesaemia, and hypophosphatemia as these can quickly worsen when switching metabolism back to an insulin secretion state.
- Mixed metabolic disorders are common as a result of ketoacidosis alongside vomiting or hyperventilation leading to alkalosis as well.
- Don’t forget the thiamine
Author:
Hakkam Zaghmout, MD MSc
Peer Reviewed and Edited By:
Timothy Stokes, MD


You must be logged in to post a comment.