A 35 year old male with no PMH presents for SOB. On arrival, the patient is in respiratory distress and is unable to provide any additional history to you. He is 80% on room air with a RR of 29. BP is 180/90, and HR is 125. Temp by axilla is 37.5.
A portable CXR is obtained:
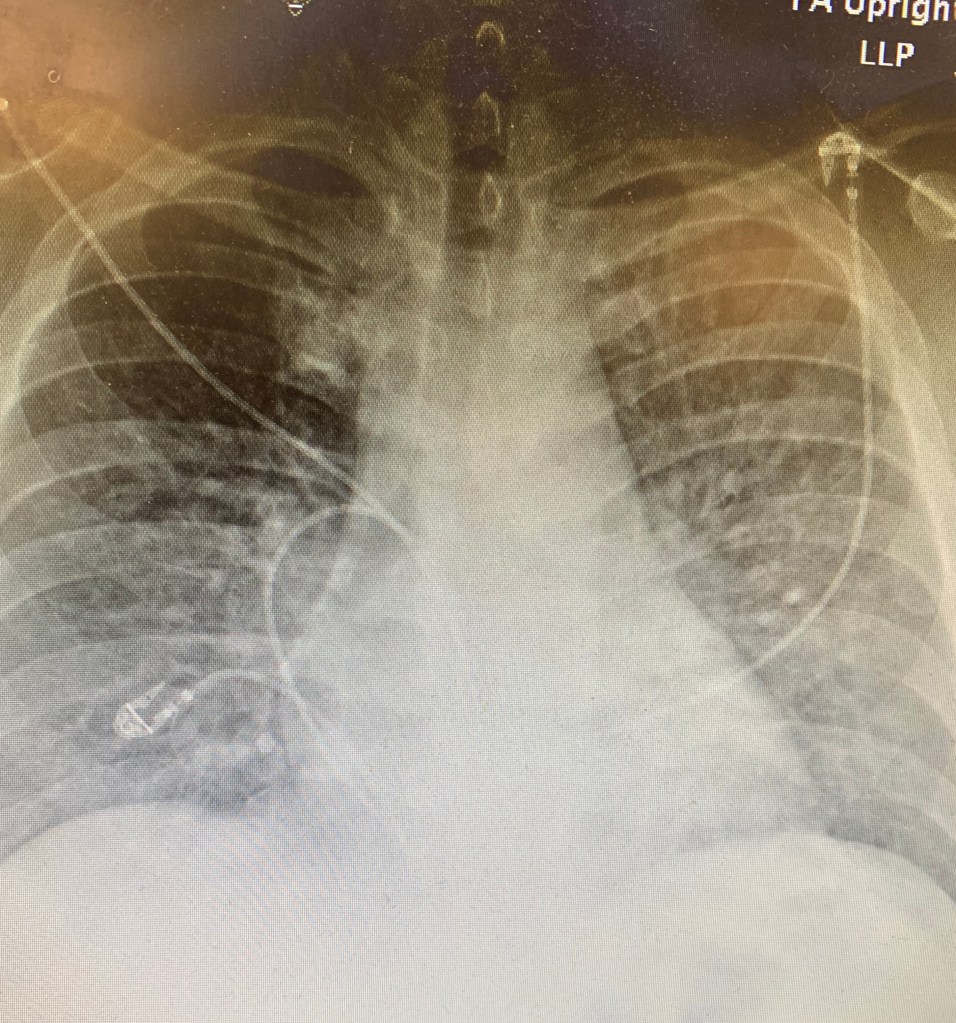
Radiology read: pulmonary edema. The patient has no cardiac history, and so a POC pulmonary and cardiac ultrasound are obtained.
Pulmonary ultrasound:
Although only two lung fields are shown above, the pulmonary ultrasound shows B lines in all lung fields.
Cardiac ultrasound:
The cardiac ultrasound shows no pericardial effusion, no right heart strain, and the EF is not decreased/the heart is actually hyperdynamic.
What is your new differential?
A CT is obtained:
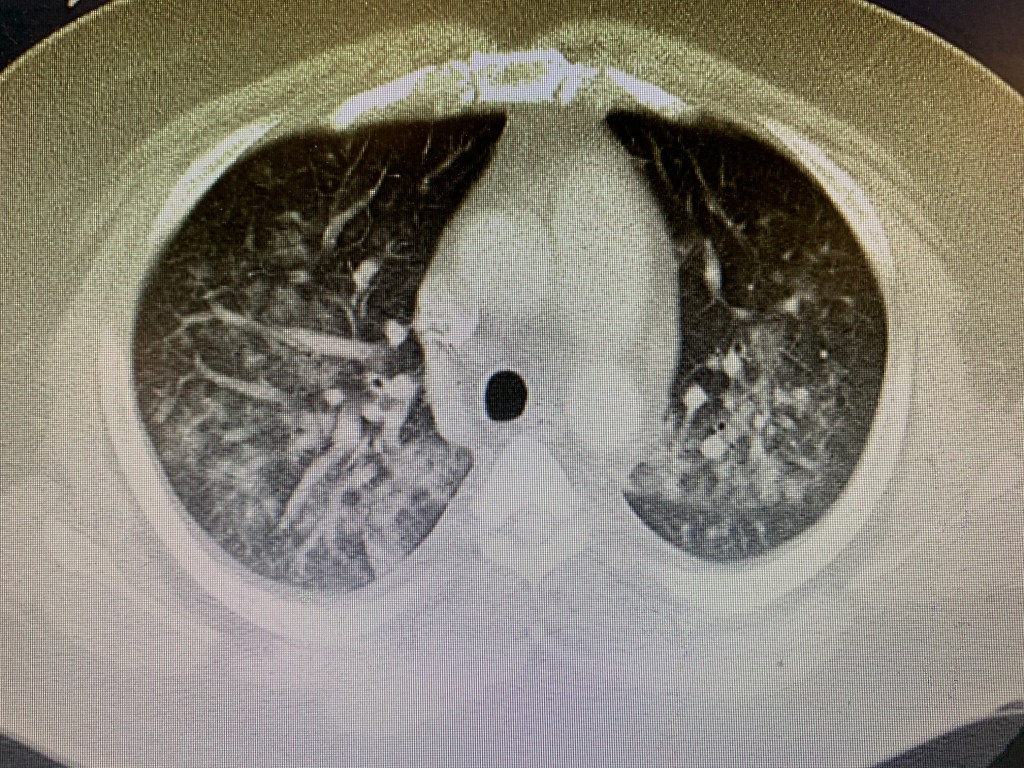
The CT shows multifocal pulmonary infiltrates diffusely throughout the bilateral lungs. An ABG is obtained on 100% FiO2 (the patient is placed on vapotherm prior to the ABG) and the PaO2/FiO2 ratio is 150. The patient is diagnosed with ARDS and multifocal pneumonia and admitted to the ICU.
Case wrap up:
The patient had a CXR concerning for pulmonary edema (but retrospectively it was actually bilateral interstitial opacities or non cardiogenic pulmonary edema consistent with ARDS) with an echo that showed a hyperdynamic heart and a pulmonary ultrasound that showed diffuse b lines in all fields. CT confirmed the diagnosis of diffuse alveolar opacities/pneumonia. The patient did not have heart failure, but rather had sepsis secondary to pneumonia/ARDS.
Remember that B lines do not necessarily mean fluid, they just mean not air. They can be signifying fluid, blood, pus, fibrosis, etc. It is up to you to put together their distribution and the patient’s clinical picture to decide what they most likely mean.
Also remember that to be a true B line, the line needs to go down to 18cm, and there should be at least three in the lung field you are examining. They also should obliterate any a lines in the field.
The patient ended up having leukocytosis, lactic acidosis, and when core temp was obtained he had a fever. He had a prolonged ICU course but did not require intubation and slowly improved on vaoptherm and broad spectrum abx. All testing for rarer causes of pneumonia were negative (fungal, strep, legionella, etc).
Take home points:
- Not all B lines are pulmonary edema
- B lines can signify blood, pus, edema, atelectasis, etc
- Pair an echo with pulmonary ultrasound and the clinical picture to guide resuscitation and narrow your differential


You must be logged in to post a comment.