A 76 year old woman presents to the ED with progressive leg weakness. The patient states that for several days she’s been having trouble standing from a seated position, and has had multiple falls recently. PMH includes HTN, COPD, neuropathy and chronic hyponatremia (etiology not stated in records).
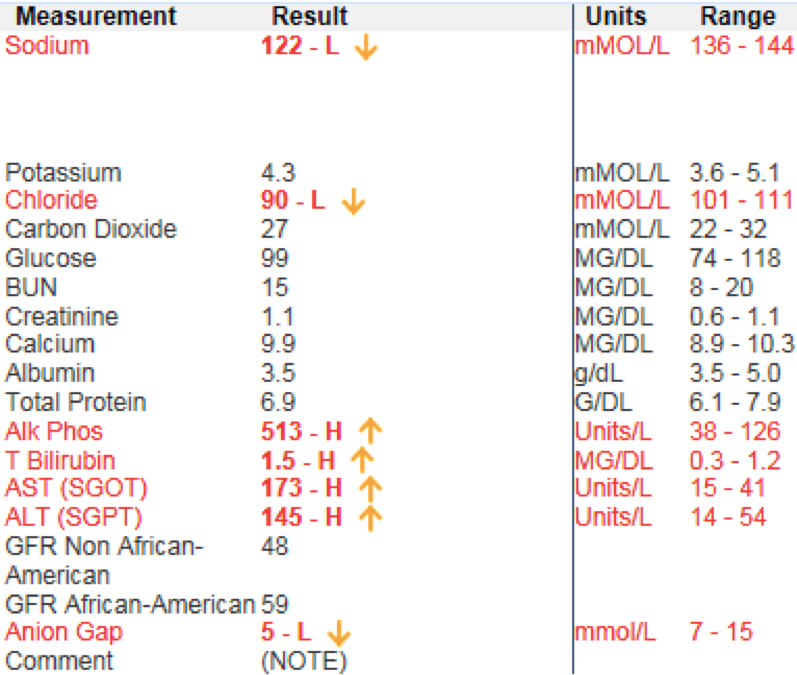
The patient states that for years she has been told her sodium was low and has been admitted to the hospital before, but has yet to know why her sodium is low. Initial workup included a CBC/CMP, showing the following:
Categorizing hyponatremia
Hypotonic hyponatremia (the most common one we will see in the ED) falls into three categories which aid in identification and management. These categories are based on a patient’s volume status, with further categorization regarding duration and severity:
Hypovolemic Hyponatremia
These patients are clinically dehydrated presenting with vomiting, diarrhea, burns, renal tubular acidosis or renal loss. These patient’s management should include IV fluids along with treatment of underlying pathology.
Hypervolemic Hyponatremia
These patients have a decrease in their free water excretion presenting with renal failure, congestive heart failure, or liver failure. These patients tend to need volume restriction and loop diuretics (as well as treatment of the underlying etiology).
Euvolemic hyponatremia
Patients with euvolemic hyponatremia may present as a result of psychogenic polydipsia, beer potomania, medication side effect, SIADH, tea/toast diet, thyroid dysfunction and many other etiologies. Management of euvolemic hyponatremia includes fluid restriction along with treating the underlying disorder.
Duration
Acute: Period of less than 48 hours, generally seen in parenteral fluid administration for post operative patients and self induced water intoxication. Also seen in runners, polydipsia, and users of ecstasy.
Chronic: > 48 hours or unknown duration
Severity
Symptomatic hyponatremia can present as fatigue, nausea, dizziness, vomiting, gait disturbances, forgetfulness, confusion, lethargy and muscle cramps.
Na level:
Mild: 130 to 134 mEq/L
Moderate: 120-129 mEq/L
Severe: <120 mEq
Treatment:
Treatment is dictated by several factors such as acute/chronic, euvolemic/hypovolemic/hypervolemic, and mild/moderate/severe indicating an importance to treat the underlying cause appropriately as opposed to the sodium value in a hospital setting. Initial management however is as follows:
Acute Hyponatremia (less commonly seen)
- Asymptomatic
- <130 mEq/L is treated with 50 mL bolus of 3% saline.
- The reason being that patients presenting with self induced water intoxication may continue to decline as a result of delayed water absorption
- Symptomatic
- <130 mEq/L is treated with 100 mL bolus of 3% saline over the course of ten minutes with 2 additional 100 mL bolus in the event of continued symptoms.
- Possible symptoms include nausea, vomiting, tremors, headache, coma, seizures, respiratory arrest, gait or movement disturbances, or confusion.
Chronic Hyponatremia (more commonly seen)
- Asymptomatic, mild, moderate
- Does not require hypertonic saline. Admission to hospital depending more so on clinical presentation
- Severe (<120 mEq/L)
- 3 percent saline at rate of 15 to 30 ml/hr. Along with this, patients with corrected hypovolemia can potentially develop water diuresis during therapy and as a result, desmopressin should also be administered
- 1 to 2 mcg every 6 to 8 hours for 24 to 48 hours or until serum sodium increases to ≥125 mEq/L. Restrict water intake.
- 3 percent saline at rate of 15 to 30 ml/hr. Along with this, patients with corrected hypovolemia can potentially develop water diuresis during therapy and as a result, desmopressin should also be administered
Isotonic saline should be avoided in true volume depletion as it raised sodium by 1 mEq for every liter of fluid, and by correcting hypovolemia the stimulus on ADH is removed, leading to excess urine excretion
Central Pontine Myelinolysis
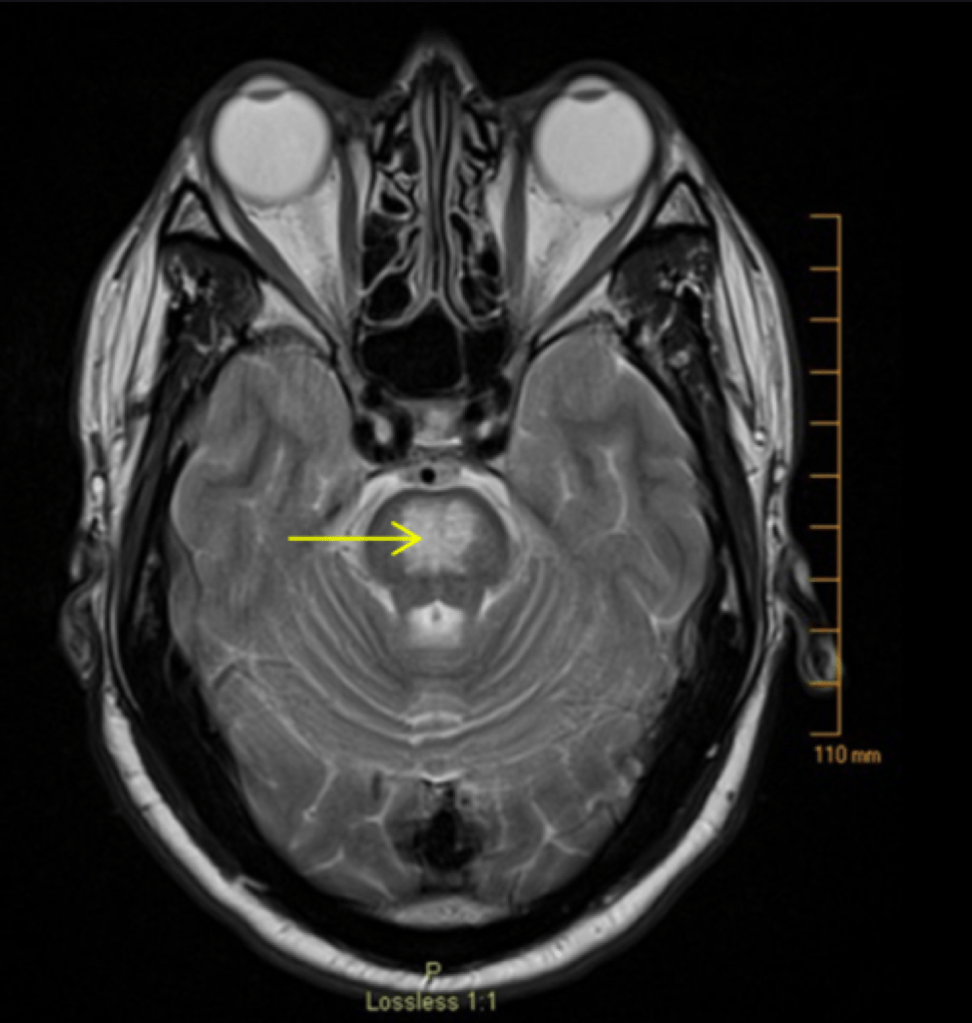
Otherwise known as osmotic demyelination syndrome, central pontine myelinolysis is a focal demyelination in pons/extra pontine area leading to neurologic dysfunction. Decrease in serum tonicity causes water to flow across the blood brain barrier, effectively increasing water content of the brain.
The clinical presentation of central pontine myelinolysis is delayed 2-6 days following a rapid elevation in sodium concentration with symptoms such as dysarthria, dysphagia, para/quadraperesis, behavioral disturbances, seizures, confusion, obtundation, coma, with severe cases leading to locked in syndrome.
- Risk factors for central pontine myelinolysis
- <105 mEq/L
- Concurrent hypokalemia
- Chronic alcohol intake
- Acute/Chronic hepatic disease
- Malnourishment
Case Conclusion
Initially patient stated that she was a casual drinker. Looking again at the CMP, the patient appeared to have an elevated MCV, AST and ALT. The patient was once again prompted regarding her drinking status and stated that she in fact was a daily drinker (6-8 drinks a day), thus placing the possible etiology of hyponatremia as beer potomania.
Attending Commentary
Using hypertonic saline boluses (3%) in non symptomatic patients or patients with mild symptoms and Na >120mEq will tend to raise eyebrows. The physiology of why UpToDate recommends hypertonic saline in almost all cases if not fluid restricting is because it offers a more predictable rise in the Na and should not inhibit ADH as much as isotonic saline, theoretically avoiding free water loss and rapid over correction. Many hospitals however can not use hypertonic saline as treatment of hyponatremia in non ICU patients. A more standard approach to non hyper acute patients (different population all together and not what we commonly seen) follows.
Na <120mEq with symptoms:
This is not really in debate in the literature. If you have severe hyponatremia and you have any symptoms you should be treating with hypertonic saline. The safest way to do this is to put in a foley, give ddAVP (to prevent free water loss and over correction), and give 100ml 3% boluses up to 3 times total until symptoms resolve.
Na <120mEq without symptoms:
There is an option to use 3% here, however many people will not if there are no symptoms at all. What you should do however is put in a foley to ensure you are not getting rapid free water loss (you will see patients all of a sudden dump liters of urine sometimes), give ddAVP to try to prevent over correction, and use isotonic fluid at a calculated rate (use a medical calculator) to raise Na slowly. These patients need to be in an ICU.
Na >120mEq
If hypovolemic, do not give fluid boluses unless the patient is hypotensive/emergently needs boluses for stabilization. Instead, calculate the rate of isotonic fluid administration needed to raise the Na appropriately and slowly. If hypervolemic, fluid restrict and consider Lasix as well as optimizing the underlying disease process. If euvolemic, fluid restrict and target therapy to the underlying disorder.
In all these patients, watch closely for excess urine excretion which is signifying too much ADH suppression and rapid free water loss. If this starts to happen, give ddAVP to prevent over correction.
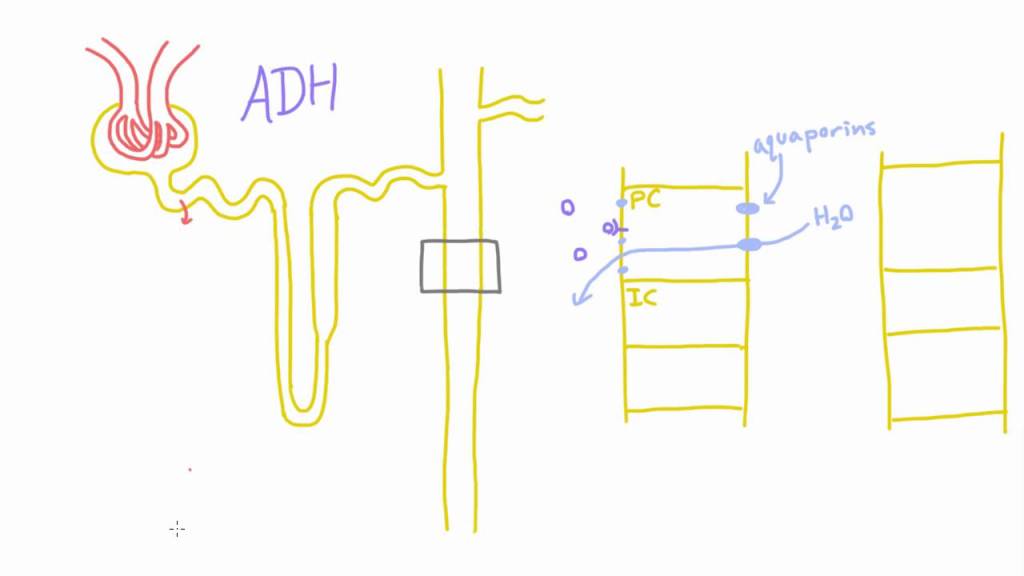
What’s the deal with ddAVP?
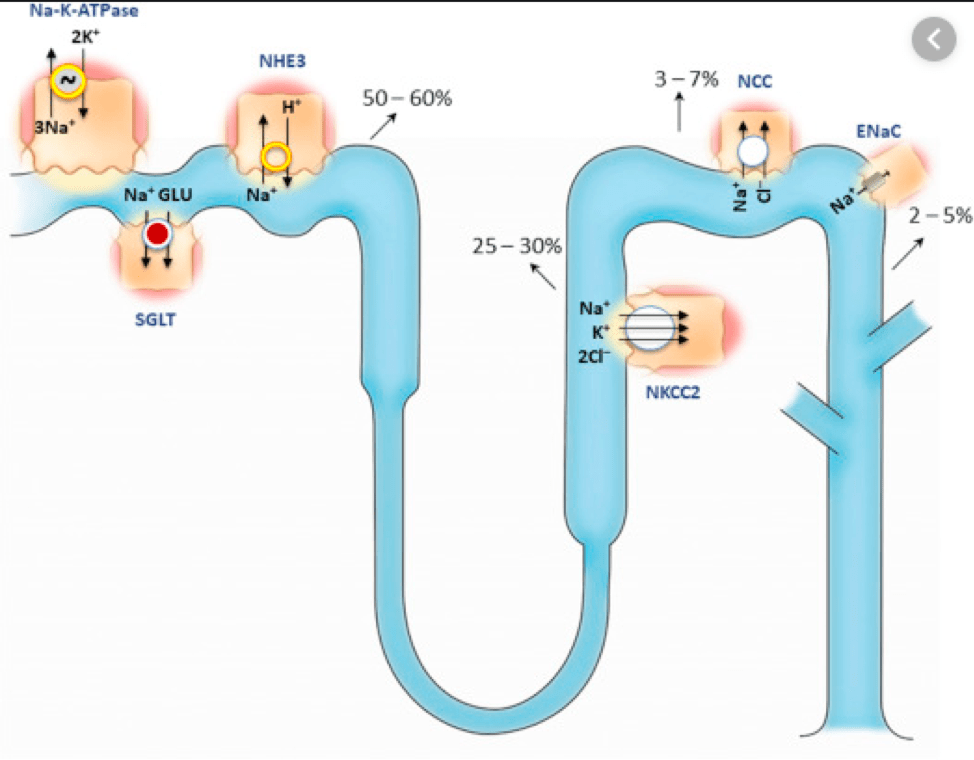
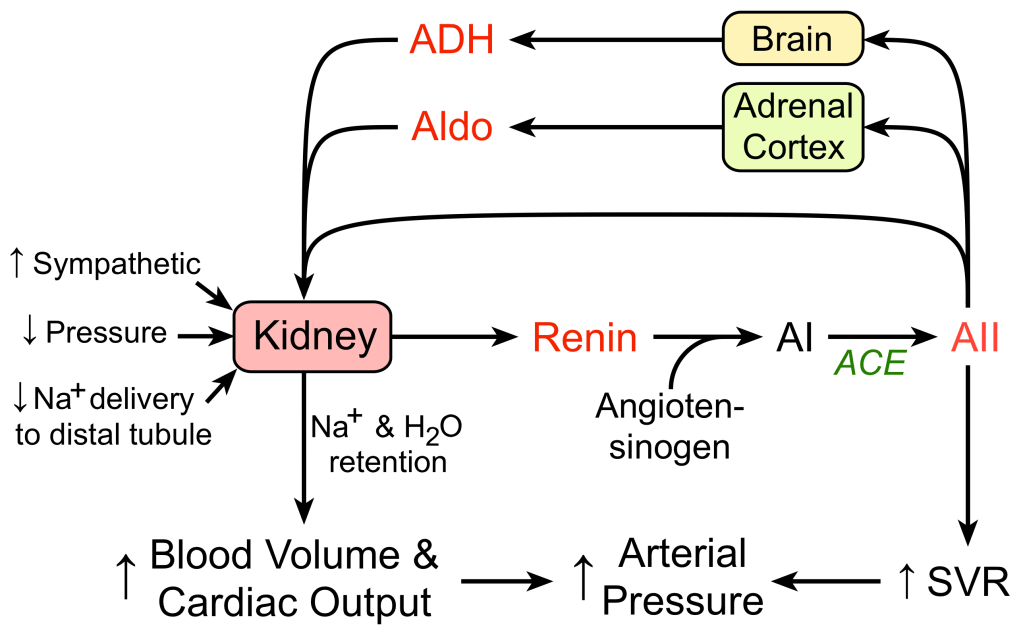
Patients who are hypovolemic will have high ADH activity. Remember ADH is linked to the renin angiotensin aldosterone pathway. If you are hypovolemic (or have low effective circulating volume), the RAAS pathway will be ramped up and ADH will attempt to stimulate free water reabsorption to attempt to increase your circulating volume. If you start to bolus patients who have hypovolemia and hyponatremia, you will rapidly suppress the RAAS and ADH. This will lead to large volume free water elimination and rapid loss of free water (you will create lots of dilute urine). If left unchecked, this can lead to accidental Na overcorrection.
One way to prevent over correction is to just empirically give ddAVP. This will prevent suppression of ADH and prevent the creation of dilute urine. Essentially you are creating a “fixed tank” in the body and are attempting to suppress the patient’s creation of urine. You are trying to be in complete control of the Na level and allow the fluids you are administering to cause a predictable rise in Na.
What’s the deal with over correction?
The goal of initial therapy for emergent correction of hyponatremia is to raise the serum sodium concentration by 4 to 6 mEq/L in a 24 hour period. In patients who require emergency therapy, this goal should be achieved quickly, over 6 hours or less with the serum sodium concentration being maintained at a constant level thereafter. Do not exceed 8 mEq/L in a 24 hour period.
A 4 to 6 mEq/L increase in serum sodium concentration appeasr to be sufficient to reverse the severe manifestations of hyponatremia. We do not want to exceed 8 mEq/L in a 24 hour period because of the fear of causing osmotic demyelination syndrome – a neurologically devastating condition related to the rapid correction of hyponatremia. Most cases of ODS have occurred in patients with severe hyponatremia whose serum sodium concentration was raised by more than 10 to 12 mEq/L in a 24 hour period, although there have been cases reported of this occurring even at slower correction rates of 9 mEq/L in 24 hours. The 24 hour goal may be achieved in the first few hours as it is the daily change, rather than the hourly change, that is associated with osmotic demyelination.
What if I overcorrect?
Relower the sodium!
Relowering the serum sodium can reverse the breakdown of the blood-brain barrier that occurs with rapid correction and can prevent the infiltration of microglia that is a feature of osmotic demyelination. Because it is not the hourly change that matters but the daily change over 24 hours, by lowering the sodium back to an acceptable range of 8 mEq/L from the initial sodium, you can help to prevent ODS. In patients who you accidentally overcorrect, perform the D5W/ddAVP rescue to try to bring them back into the range of proper correction.
D5W/ddAVP rescue:
D5W 6mL/kg ideal body weight infused over 2 hours
dDAVP 2mcg IV q6hr
This should lower the sodium by approximately 2meq/L every 2 hours. Check serum sodium q2hr to ensure you are not overshooting your goal and that the patient is correcting appropriately. Once goal sodium achieved, the D5W is stopped but the ddAVP is continued to prevent overly rapid correction.
Take away points:
- Identify volume status, acute vs. chronic and severity to tailor your treatment.
- Symptomatic severe hyponatremia can be treated by 100 mL bolus of 3% hypertonic saline at rate of 10 minutes up to three times.
- Correction of sodium should be 4-6 mEq per day, with correction exceeding 8 causing an increased risk of central pontine myelinolysis.
- Do not administer fluid boluses to your patients with severe hyponatremia unless they emergently need them. Calculate the rate of fluid needed for appropriate slow correction.
- Sometimes with hyponatremia, the most you can do for your patient is to do nothing and just fluid restrict until the etiology is known.
Authors:
Hakkam Zaghmout, MD
Peer reviewed and edited by:
Timothy Stokes, MD


You must be logged in to post a comment.