Often times when presenting a patient as an intern, we’ll feel that our attending is being a tad overzealous. Is it possible this man with back pain has an aortic dissection? Yes, it is. Is it out of the realm of possibilities? Just about. However here is a case that plays homage to the classic saying regarding aortic dissections, “Unless your index of suspicion is high, you’ll never catch it.”
58 y/o man presents to the ED by EMS appearing acutely agitated with left foot pain. At arrival patient was diaphoretic, anxious, combative and unable to provide detailed history due to pain. Patient states that prior to arrival he walked into his bathroom and suddenly had an unbearable pain in his toe. PMH includes HTN for which patient is non compliant with medication.
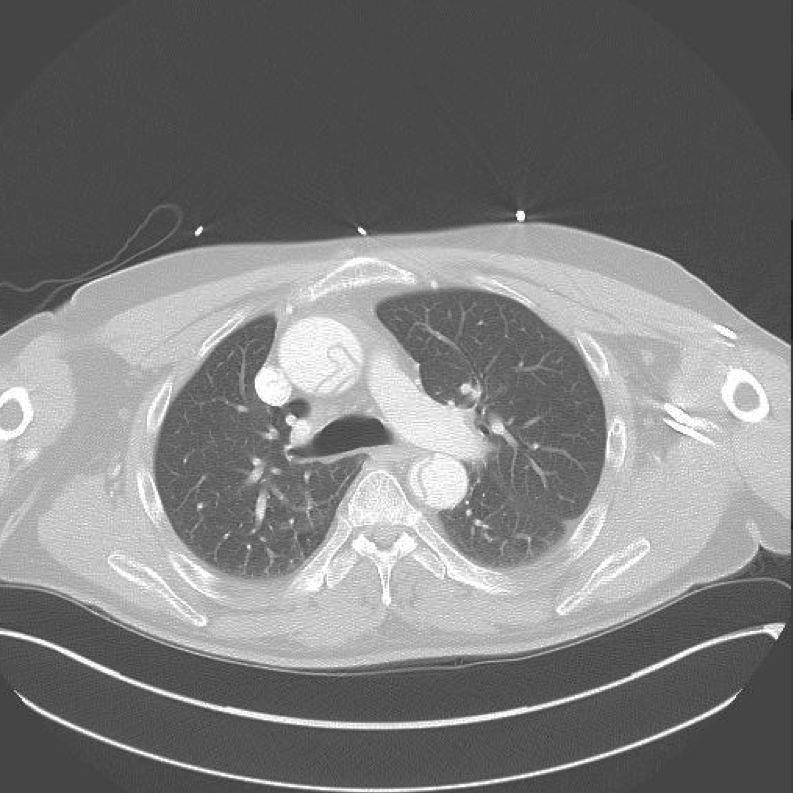
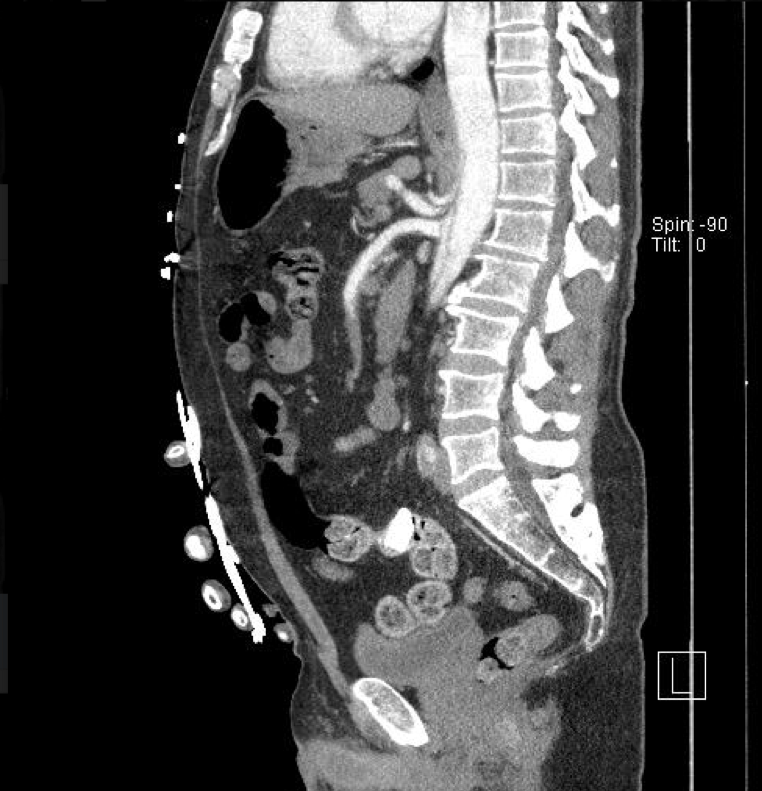
At initial evaluation, patient appeared to not have pulses on his left leg including dorsalis pedis, posterior tibialis, popliteal artery and femoral artery. Seconds following the initial evaluation, patient began to state he was having chest pain. CT of chest/abdomen/pelvis with run off was ordered, and the results immediately evident:
Aortic Dissection:
An aortic dissection is when the aorta begins to bleed into the intimal tear, separating the intima from the media and adventitia. As the blood continues to accumulate into this false lumen, the tear extends leading to a separation of the layers.
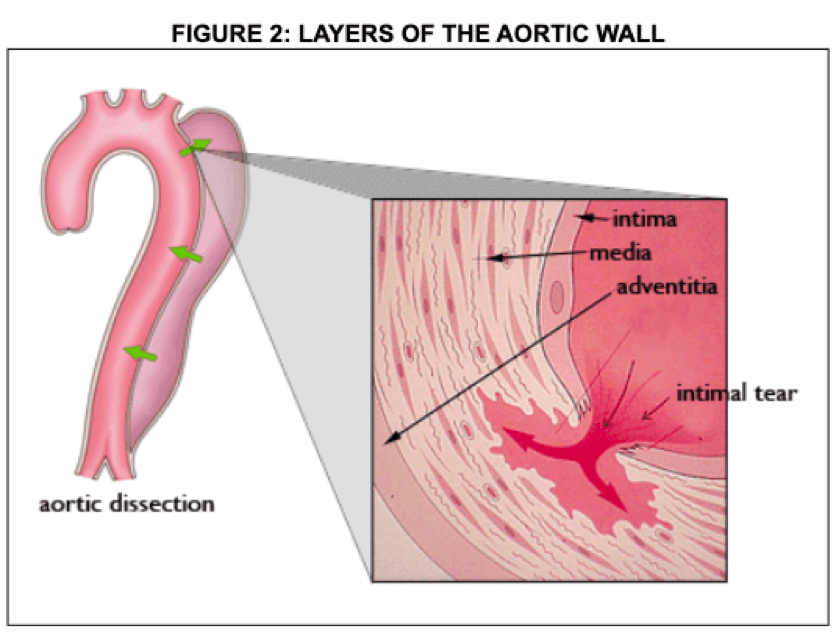
Risk factors for aortic dissections include hypertension, and a myriad of genetic diseases such as Marfan syndrome, Ehlers-Danlos syndrome, Turner syndrome, and Osteoarthritis. Risk factors also include cardiac abnormalities such as aortic aneurysms, bicuspid aortic valve, pre-existing TAA and coarctation.
50-65% of intimal tears originate in the ascending aorta, with 20-30% of tears originating near the left subclavian with extension to thoracic and abdominal aorta. Extension proximally and distal from initial tear will lead to clinical complications such as aortic regurgitation, cardiac tamponade, coronary/cerebral ischemia, and in our case a kidney infarction as seen by image 1.
Patients classically present as men with an average age of 67 years old with chest or back pain. In fact, in over 90 percent of patients with an aortic dissection chest/back pain was reported, with 85% stating that pain was abrupt in nature. Patient’s also present with absent pulses, heart murmur, focal neurologic deficits, syncope, and hypotension.
Classification
There are two methods of classification regarding aortic dissections, Stanford and Debakey. Stanford is the most often used of these two classification systems. Stanford classification involves location of dissection regardless of origin of tear, with Debakey involving origin. Stanford Type A is a surgical emergency that classifies a dissection involving the ascending aorta, with Stanford Type B indicating the descending aorta. Debakey type I indicates tear originating in ascending aorta and involves both the ascending and descending aorta.. Type II remains confined to the ascending aorta and type III originates in the descending aorta with extension distally or proximally.

- Classification also includes:
- aortic intramural hematoma
- intimal tear without hematoma
- penetrating atherslerotic ulcer
- Etiology
- Sporadic
- Genetically Mediated
- Traumatic
Mortality of aortic dissection appears to be 20-30% at initial presentation, with 10 year mortality between 30-88% following discharge from hospital.
Management
Initial management is centered around hemodynamic stability with large bore IV access and a focus on maintaining a blood pressure below 120/80. Hypertension initial medication treatment involves anti impulse therapy with esmolol 0.1 to 0.5 mg/kg IV bolus followed by 0.02 to 0.2 mg/kg/min or labetalol 20 mg IV with additional options of diltiazem or verapamil. The goal is a HR less than 60. In the necessity of further medication, first line vasodilators such as nitroprusside and nicardipine should be used to bring the blood pressure to a goal below 120/80.
Vascular or thoracic surgery must be emergently consulted in order to determine whether surgical intervention is deemed necessary.
Discussion
Following our CT of the chest/abdomen/pelvis, it became apparent that our patient’s aorta had dissected through the ICA, subclavian, SMA, to the left Iliac artery, including an infarction of the left kidney. Initial medication included Labetalol, esmolol, nicardipine with propofol also aiding in blood pressure management following intubation due to airway compromise. The patient underwent emergent surgery and survived.
With chest pain being the most common ED chief complaint, and being a reported symptom in 90% of patients with an aortic dissection, the necessity to have a high degree of suspicion remains high. An axiom in Emergency medicine is that chest pain with any neurologic deficit or complaint, one must consider aortic dissection. Initial management includes labetalol, esmolol for anti impulse therapy, followed by vasodilators such as nitroprusside and nicardipine for further blood pressure control.
Take Home Points
- Urgent need to decrease shearing forces by managing blood pressure to less than 120/80,
- Surgical intervention for Stanford Type A/Debakey I & II.
- Watch for potential clinical complications such as coronary/cranial ischemia, aortic regurgitation, cardiac tamponade.
- High index of suspicion is necessary to diagnose in a timely fashion.
Authors:
Hakkam Zaghmout, MD
Peer reviewed and edited by:
James Bohan, MD