A 69 y/o female presents via EMS with altered mental status. The patient is able to tell you her name, but can’t answer any other questions. Her husband states that she has cirrhosis and recently has been having increasing ascites as well as anorexia. She has not been compliant with her lactulose. On exam she has sequela of cirrhosis including marked ascites as well as a flapping tremor. Workup is pertinent for worsening LFTs including bilirubin and coags, as well as a creatinine that is markedly elevated above her baseline. Other than hepatic encephalopathy, you are also concerned for hepatorenal syndrome in this patient.
What is Hepatorenal Syndrome?
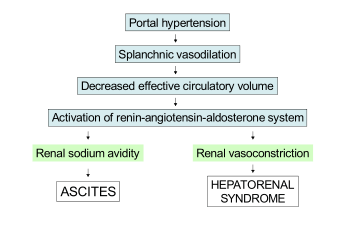
Hepatorenal syndrome is a cascade of events that lead to acute renal failure secondary to cirrhosis. The mechanism is not fully understood, but is generally thought to be caused by splanchnic vasodilation and portal hypertension. Increased portal hypertension leads to significant splanchnic vasodilation, which decreases glomerular filtration rate. This leads to severe renal vasoconstriction which further decreases GFR. This can be triggered by many things including SBP, portal vein thrombosis, and acute worsening of liver function.
How is Hepatorenal Syndrome diagnosed?
Hepatorenal syndrome is a diagnosis of exclusion for patients with known cirrhosis who have an acute decrease in GFR not explained by another etiology. In general it is a clinical diagnosis for renal dysfunction in the setting of cirrhosis not explained by something else. The diagnosis of hepatorenal syndrome is broken down into two types:
- Type 1 hepatorenal syndrome is the more severe form. It is defined by a doubling of the creatinine to at least 2.5 mg/dL within 2 weeks and oliguria.
- Type 2 hepatorenal syndrome is broadly defined as renal impairment that is less severe and does not meet the criteria for type 1. Type 2 is generally a slower, more progressive change, while type 1 is an acute deterioration.

Treatment
The definitive treatment for hepatorenal syndrome is improvement in liver function/optimizing cirrhosis treatment. This can be from abstinence from alcohol, appropriate treatment for viral hepatitis, or in certain cases liver transplant. In addition, dialysis can be indicated for patients as a bridge to liver transplant or until improvement in liver function is achieved.
In the acute setting, the goal is to improve perfusion to the kidneys to prevent mortality and worsening renal decompensation.
Critically ill patients:
- Norepinephrine is used to raise the MAP by at least 10 mmHg even if the patient is not hypotensive. The thought is that even if not hypotensive, the kidneys are not receiving enough perfusion as indicated by the decrease in GFR because of the mechanisms explained above.
- Albumin at 1g/kg/day (max 100g) for at least 2 days. This is a very large dose of albumin and not the typical 12.5-25g that is sometimes given in the ED.
Non critically ill patients:
- Midodrine is used TID for a similar reason as norepinephrine
- Octreotide infusion is used to decrease portal hypertension
- Albumin at 1g/kg/day (max 100g)
In addition, all patients with hepatorenal syndrome and either confusion or abdominal pain should undergo a diagnostic paracentesis to exclude SBP as this is a frequent precipitant of hepatorenal syndrome.
Prognosis
Patient’s with hepatorenal syndrome are very sick. Trials comparing different vasoconstrictors for the treatment of type 1 hepatorenal syndrome report 30 day survival rates of about 40% with maximal medical therapy. The only definitive treatment is liver transplantation, but these patients are rarely good candidates. Given the high mortality rate, it is imperative that we recognize this diagnosis and aggressively treat it.
Take home points:
- Hepatorenal syndrome is a diagnosis with high mortality rates and must be recognized and treated aggressively.
- Consider this is anyone with cirrhosis and an acutely elevated Cr not obviously explained by another etiology.
- Have a very low threshold in these patients to perform a diagnostic paracentesis.
- In the ED, initiate norepinephrine and high dose albumin if the patient is critically ill (even if not hypotensive), and if not critically ill start high dose albumin, midodrine, and an octreotide drip.
Authors:
Timothy Fields, MD
Peer reviewed and edited by:
Timothy Stokes, MD

