On a bright sunny morning, a 55 y.o. male uncomfortably staggers into the ED. He is escorted by his cardiac rehab nurse who notifies the ER staff that the patient had a recent cardiac stent placed in the proximal LAD. The patient had chest pain earlier in the day at cardiac rehab that progressively became worse. The pain is substernal and is associated w/ some SOB.
On exam, he was glistening with sweat and was very diaphoretic. VS were stable with O2 Sat at 99% RA. Lungs were CTAB. Good pulses bilaterally. RRR. No harsh murmurs. CXR normal.
EKG:
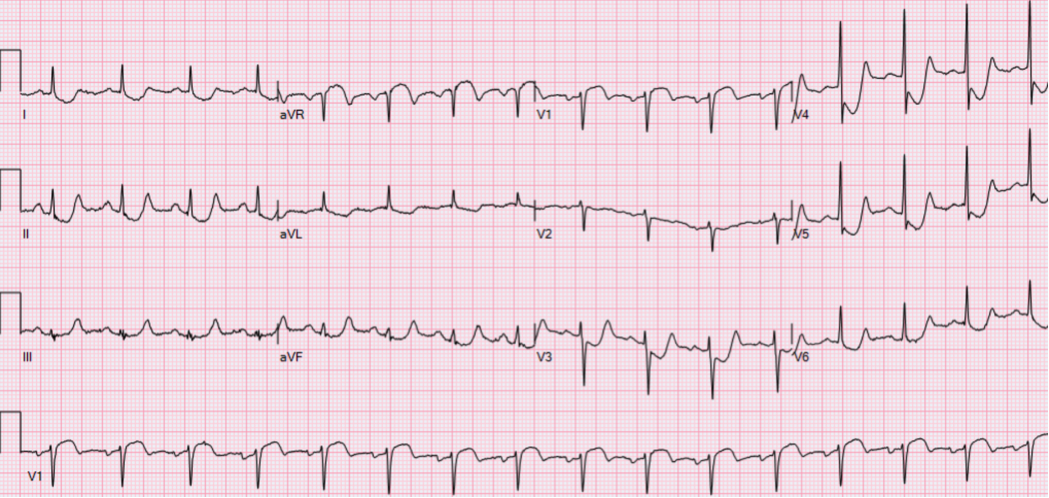
Significant EKG Findings:
- ST elevation in aVR
- ST elevation in V1 of equivalent height
- Diffuse ST depressions in other leads
Based on the history, exam, and EKG, the patient was taken emergently to the cath lab and had an Ostial LAD stent placed for an obstructing culprit lesion.
Elevations in aVR
ECG findings with Left main coronary artery (LMCA) occlusion:
- Widespread horizontal ST depression, most prominent in leads I, II and V4-6
- ST elevation in aVR ≥ 1mm
- ST elevation in aVR ≥ V1 (predicts LMCA occlusion over prox LAD)
ST Elevation in aVR may also be seen with:
- Proximal left anterior descending artery (LAD) occlusion
- Severe triple-vessel disease
- Diffuse subendocardial ischemia – ex: following resuscitation from cardiac arrest
Mechanism of ST elevation (STE) in aVR
- Lead aVR is electrically opposite to the left-sided leads I, II, aVL and V4-6; therefore, ST depression in these leads will produce reciprocal ST elevation in aVR.
- Lead aVR also directly records electrical activity from the right upper portion of the heart, including the right ventricular outflow tract and the basal portion of the interventricular septum. Infarction in this area could theoretically produce ST elevation in aVR.
Predictive Value of STE in aVR
In the context of widespread ST depression + symptoms of myocardial ischemia:
- STE in aVR ≥ 1mm indicates proximal LAD / LMCA occlusion or severe 3VD
- STE in aVR ≥ 1mm predicts the need for CABG
- STE in aVR ≥ V1 differentiates LMCA from proximal LAD occlusion
- Absence of ST elevation in aVR almost entirely excludes a significant LMCA lesion
In the context of anterior STEMI:
- STE in aVR ≥ 1mm is highly specific for LAD occlusion proximal to the first septal branch
In patients undergoing exercise stress testing:
- STE of ≥ 1mm in aVR during exercise stress testing predicts LMCA or ostial LAD stenosis
Magnitude of ST elevation in aVR is correlated with mortality in patients with acute coronary syndromes:
- STE in aVR ≥ 0.5mm was associated with a 4-fold increase in mortality
- STE in aVR ≥ 1mm was associated with a 6- to 7-fold increase in mortality
- STE in aVR ≥ 1.5mm has been associated with mortalities ranging from 20-75%
LMCA Mimics
Tachycardia-Related ST Depression
Widespread ST depression (with reciprocal STE in aVR) is a common finding in patients with supraventricular tachycardias such as AVNRT or atrial flutter. The significance of this finding in individual patients is unclear, and may be due to:
- Rate-related ischemia (O2 demand > supply)
- Unmasking of underlying coronary artery disease (i.e. tachycardia as a “stress test”)
- A pure electrical phenomenon (e.g. the young patient with SVT who is relatively asymptomatic and has normal coronary arteries)
ECGs taken following reversion to sinus rhythm will usually show resolution of the ST depression. I would be concerned about underlying coronary artery disease in the following situations:
- ST depression that persists after reversion to sinus rhythm
- Signs of clinical instability – severe chest pain with diaphoresis, hypotension, syncope
- Elevated cardiac biomarkers, with delta troponin rise (NB. a small troponin leak with SVT is common and probably not significant)
- Older patient, multiple cardiac risk factors
Authors:
Sumayyha Yousufi, DO
Peer reviewed and edited by:
James Bohan, MD

