A 75 y.o m not on blood thinners presents for epistaxis. He states that for the last 2 hours, he has had bleeding from his bilateral anterior nares. He attempted to hold pressure at home without resolution. He feels a slight trickle of blood down his posterior pharynx, but denies any difficulty breathing or speaking. No trauma. States he gets epistaxis seasonally with the dry weather.
Epistaxis
Anatomy:

Physical Exam:

- Rest the speculum against the ala of the nose while pushing it out slightly and not against the septum. Once done with the examination, don’t close the speculum completely inside the nare as hairs can get caught and cause discomfort to the patient
- Can also use an otoscope if a speculum is not available
- If available, a head lamp will help illuminate your field of vision without your head obstructing your beam of light.
- Look for oozing or a visible bright red superficial vessel as possible source of epistaxis
- May need to postpone direct visualization until bleeding is controlled
- Don’t forget to examine the oropharynx to see if there are signs of posterior bleeding
Treatment:
Step wise approach (the Arango method)
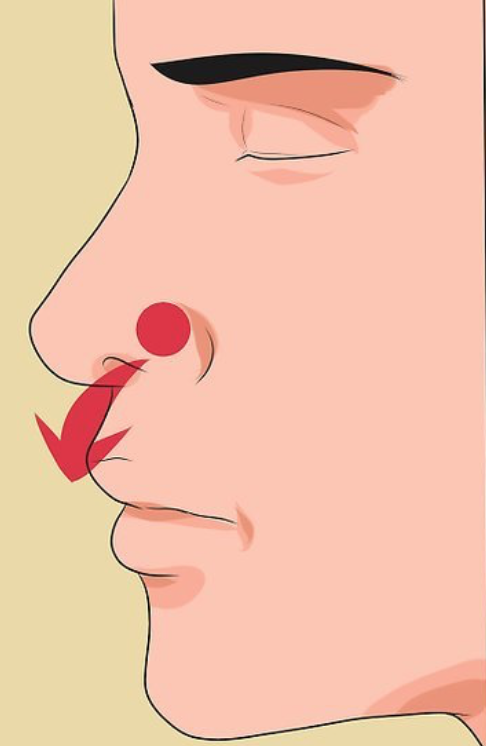
- Apply direct pressure by pinching the alae against the septum for 10-20 minutes
- Do NOT apply pressure higher up at the septum. This is ineffective
- Move on to topical therapy
- Have the patient blow their nose in order to evacuate any clot that could obstruct topical therapy
- A topical vasoconstrictor such as oxymetazoline (Afrin) can be sprayed into each nare. After applying topical therapy, reapply pressure for 10-20 minutes.
- If Afrin fails or as an alternative agent, topical use of the tranexamic acid (500mg in 5mL soaked pledget) or topical cocaine can be used
- Silver nitrate cautery
- Cautery is completed by applying a silver nitrate stick to the bleeding site for 5-7 seconds max, then applying surgical or bacitracin ointment.
- This can not be used if there continues to be brisk bleeding
- If there is oozing, start the cautery just next to the oozing site and slowly roll the silver nitrate stick to the edge of the oozing area and then across it (if the tip gets saturated with blood it will not work)
- Nasal packing
- Anterior epistaxis
- Packing is performed commonly with the Rapid Rhino or Merocel packing (for Merocel smear on antibiotic ointment, insert it horizontally)
- Apply the packing and then observe for resolution of the bleeding
- With brisk anterior bleeding, the packing may start to push the blood down the posterior pharynx
- Anterior epistaxis


- Posterior epistaxis
- Life threatening
- Brisk, posterior pharyngeal bleeding
- May need intubation for airway control
- Nasal balloon devices
- Similar to anterior packing devices, but are longer to reach the posterior pharynx
- Brands/options include Epistat and a longer Rhino Rocket
- Insertion is the same as anterior packing, but it will be inserted farther to reach the posterior pharynx
- If nasal balloon devices are not available, a foley catheter (size 10 French) can be utilized
- Lubricate and advance the catheter until the tip and balloon are visualized in the posterior oropharynx.
- The Foley balloon is then filled with approximately 5-10cc of saline and traction is applied until the balloon sits firmly against the posterior nasal choana.
- Anterior traction is maintained with the placement of an umbilical or c-clamp at the nasal ala (appropriate application of the umbilical or c-clamp is essential to preventing the complication of pressure necrosis)
- If hemostasis is not achieved after placement of the Foley catheter, anterior nasal packing may be utilized as an adjunct.
- Patients with posterior packing are at risk for reflex bradycardia and arrhythmia due to stimulation of the posterior pharynx and need admission
- Posterior bleeds need emergent ENT consultation
- Complications from nasal packing include infection such as toxic shock syndrome and sinusitis, pain, septal necrosis, and dislodgment of packing into the patient’s airway
- Systemic antimicrobial therapy for 7-10 days — has not been shown to be much better than placebo but should be considered in immunosuppressed patients
- Packing devices must be removed within 24-72 hours so close follow up is necessary
Authors:
Noelani Candelaria, DO
Peer reviewed and edited by:
Timothy Beau Stokes, MD