The post below was reviewed and edited by the guest lecturers Dr. Wiegand and Dr. Nacca from the University of Rochester toxicology department.
Flumazenil is a nonspecific competitive antagonist of the benzodiazepine receptor, which can be used to reverse benzodiazepine-induced sedation following general anesthesia, procedural sedation, or overdose. However, the use of flumazenil in the setting of overdose remains controversial, with the main concern being precipitated withdrawal seizures in patients who have developed a tolerance to benzodiazepines through chronic use or abuse. The main benefit of flumazenil is to avoid the need for unnecessary procedures, such as endotracheal intubation, CT imaging, or lumbar puncture if the patient’s mental status returns to normal after sedative effects are reversed.
During my toxicology rotation with Dr. Timothy Wiegand I gave flumazenil several times, at low doses, in chronic users without precipitating seizures. The best way to think about the use of flumazenil is to compare it to the use of naloxone. If naloxone is used in small doses the patient has reversal of the respiratory suppression and reversal of decreased mental status, but generally has minimal withdrawal effects. If we use high doses of naloxone we risk flash pulmonary edema and hyertensive emergency in high risk patients.

Indications:
- Rapid reversal of benzodiazepine overdose–induced coma and respiratory depression
- Postoperative or post-procedure reversal of benzodiazepine overdose
- Possible reversal of CNS depression from certain nonbenzodiazepine sedatives and hypnotics such as zolpidem [Ambien], zaleplon [Sonata], and eszopiclone [Lunesta].
- Reversal of peridoxical reaction to benzodiazepines in children
- Young children are more susceptible to respiratory depression from BZDs and less likely to be tolerant, making the use of flumazenil less concerning in the pediatric population.
Contraindications
- Known hypersensitivity to benzodiazepines.
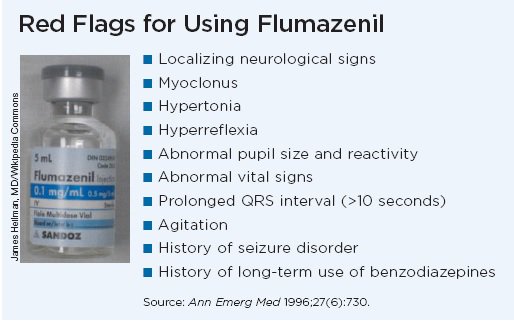
- Suspected serious tricyclic antidepressant or other proconvulsant or stimulant coingestion.
- Benzodiazepine use for control of a potentially life-threatening condition (eg,status epilepticus or increased intracranial pressure).
- Co-ingestion of another substance, such as PCP or cocaine, in which the benzodiazepine is treating the other substance ingested.
- Underlying seizure disorder
Dosing
In adults, Dr. Wiegand’s protocol is as follows: initial dose is 0.05 mg given intravenously (IV). Repeated doses of 0.05-0.1 mg, to a maximum dose of 0.1 mg if there is no noticed effect, or 0.3mg if there is a response. No more than 2 mg of flumazenil should be given within any one hour.
In children, the initial dose is 0.01 mg/kg given IV over 15 seconds or 0.05mg whichever is smaller. The initial dose may be followed at 1-2 minute intervals with up to four repeat doses of 0.005 to 0.01 mg/kg (maximum 0.05 mg) per dose.
Most sources recommend far higher doses than the above protocol, and those are the times seizures can be precipitated. The recommended doses by UpToDate and the Poisoning and Drug overdose textbook are 0.3-0.5 mg to be repeated until desired effect or a max of 3 mg. Following a protocol with lower than the commonly recommended doses Dr. Wiegand has not had any precipitated seizures in any of the patients he has given Flumazenil to.
After intravenous administration, the onset of benzodiazepine reversal occurs within 1–2 minutes with reversal peaking at 6–10 minutes, but lasting for 1–5 hours depending on the dose of flumazenil and the degree of benzodiazepine effect. It can be expected, that because we are giving a lower dose of flumazenil, the duration of action will be much shorter than what is generally reported.
Because effects last only 45min-2 hours with the lower doses, continue to monitor the patient closely for resedation. If multiple repeated doses are needed, consider a continuous infusion (0.05mg/h), especially in the case of an iatrogenic overdose or in a child.
**If flumazenil infusion is thought to be necessary, there should be a consultation with a medical toxicologist or poison control center**
Adverse effects – None of the below should be seen with low-dose flumazenil, but is important to be aware of.
- Anxiety, agitation, headache, dizziness, nausea, vomiting, tremor, and transient facial flushing.
- Flumazenil has precipitated arrhythmias in a patient with mixed benzodiazepine and chloral hydrate overdose.
- Black box warning.
- Rapid reversal of benzodiazepine effect in high-tolerance patients, such as those with benzodiazepine addiction or chronic use, especially if they have a history of seizures, may result in an acute withdrawal state, including hyperexcitability, tachycardia, and seizures.
- Seizures may be unmasked in patients with a serious tricyclic antidepressant or other proconvulsant overdose due to loss of protective effect of benzodiazepines.
Pearl: Common board question – EKG showing sinus tachycardia, QRS prolongation and a wide terminal R wave in lead aVR. You may be asked to pick from a list a medications which one is contraindicated, and among the list will be flumazenil. These are classic EKG changes of a TCA overdose, in which the removal of a benzodiazepine will almost certainly precipitate a seizure.

Take Home Points:
- If used in the correct clinical scenario, flumazenil can be an appropriate tool in the emergency department
- Consider using a low dose regimen to avoid the feared adverse effects
- Be wary of using in patients with co-ingestion or chronic use
- Many times children are appropriate candidates for flumazenil administration
Authors:
Krista Maier, DO
Peer reviewed and edited by:
Nicholas Nacca, MD
Timothy Wiegand, MD

