A 47 year-old male presents to the emergency department reporting 3 days of intermittent chest discomfort, palpitations, diarrhea, vomiting, and malaise. He has a past medical history significant for atrial fibrillation and “thyroid problems.” He states that he stopped taking all of his medications about a month ago for an unknown reason.
On arrival in the ED, the patient is conscious and alert, but speaks with a notably flat affect. His skin is pale, and he appears malnourished and older than his stated age. Initial HR 140, BP 118/78, RR 22, SpO2 100% on RA and temp 38.1 °C. Initial EKG showed afib with RVR but no STEMI. The patient’s abdominal exam was benign and his lungs were clear. CXR did not show PNA and troponin was initially negative. He did however have a free T4 of >5.60 ng/dL (normal is 0.58-1.64) and a TSH level that was undetectably low. A bedside echocardiogram was performed, which showed profound LV hypokinesis with an estimated EF of 10%. When questioned, patient denied any history of heart failure.
Thyroid Storm
Risk Factors and Causes:
- Thyroid Storm is considered the most severe and potentially life-threatening form of thyrotoxicosis
- It is usually precipitated by an acute event such as thyroid or nonthyroidal surgery, trauma, infection, an acute iodine load, or childbirth.
- Patients with known hyperthyroidism (Graves’ disease, toxic multinodular goiter, solitary toxic adenoma) are at greatest risk, but thyroid storm can also occur in normally euthyroid patients faced with any of the precipitating events mentioned above
- Irregular use or discontinuation of antithyroid treatment is also a commonly reported precipitant of thyroid storm
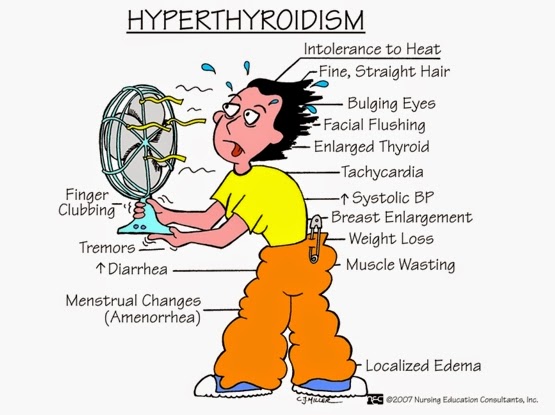
Clinical Features:
- Tachycardia
- Worsening or new-onset congestive heart failure
- Cardiogenic shock and death can result
- Cardiac arrhythmias
- Hyperpyrexia (104-106 °F is common)
- Mental status changes
- agitation, anxiety, delirium, psychosis, stupor, or coma
- although rare, apathy and flat affect can occur
- Gastrointestinal distress
- nausea, vomiting, diarrhea
- abdominal pain
- Liver failure,jaundice
Laboratory Findings:
- Most common pattern:
- ↑ T3 and/or T4
- ↓ TSH
- Other common findings:
- ↑ blood glucose
- ↑ serum calcium (mild)
- ↑ LFT’s
- ↑ or ↓ WBC
Diagnosis:
- No universally-accepted diagnostic criteria. Diagnosis is mainly clinical
- Burch-Wartofsky Point Scale (BWPS) for Thyrotoxicosis can be used to assist in diagnosis
- Diagnosis is made based on the presence of life-threatening symptoms (hyperpyrexia, cardiovascular dysfunction, mental status changes) in a patient with other laboratory findings and/or clinical features consistent with thyrotoxicosis
Treatment:
The specific medications used to treat thyroid storm may vary between institutions and providers, but the basic treatment regimen and most common therapeutic options remain fairly consistent. Treatment can be broken down into the following 4 treatment goals:
1) Control sympathetic tone with a beta-blocker
- Propranolol PO 60-80 mg q4hr
- OR
- Propranolol IV 1-2mg over 10 min; then drip at 3-5 mg/hr
- OR
- Esmolol 250-500 mcg/kg loading dose, then 50-100 mcg/kg/min
2) Block thyroid hormone synthesis with a thionamide
- PTU 600-1000 mg PO or PR followed by 200-250 mg q4hr
- OR
- Methimazole 20-25 mg q4hr
3) Block thyroid hormone release with iodine
- Potassium iodide (SSKI) 5 drops (0.25 mL or 250 mg) orally given 1 hour after PTU/Methimazole; then q6h
4) Reduce conversion of T4 to T3 with glucocorticoids
- Hydrocortisone 100-300 mg IV bolus; followed by 100 mg q8h
- OR
- Dexamethasone 4 mg IV q6h
Case Resolution:
The patient was diagnosed as having thyroid storm with afib with RVR, mental status change (flat affect/apathy), fever, vomiting, diarrhea, and CHF. It turned out that the patient had a history of Graves’ disease and had stopped taking his medications. The patient was subsequently started on an IV esmolol drip (with the patient’s severe acute CHF, we wanted to choose a medication that would quickly reverse/wear off in case the beta blocker caused decompensation), oral PTU, IV hydrocortisone, and oral potassium iodide 1 hour later. The patient was transferred to the ICU and throughout his stay with continuation of his thyroid storm “cocktail,” he continued to improve and his thyrotoxicosis resolved. Repeat echocardiogram showed a greatly improved EF after resolution of his thyroid storm.

