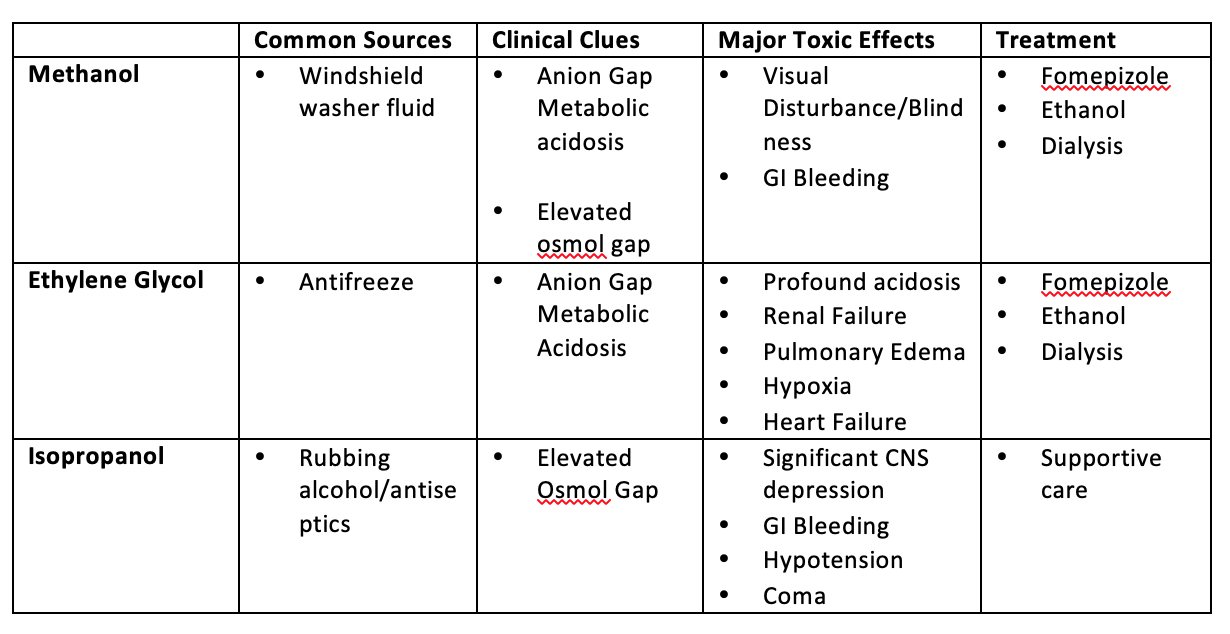
Poisonings with methanol, ethylene glycol, and isopropanol often present the emergency physician with major diagnostic challenges:
- The identity of the ingested substance is frequently a mystery on presentation.
- Patients with an intentional ingestion, either for recreation or with suicidal intent, may be less than forthcoming.
- Young patients may not be able to identify the substance.
- Patients may be in significant distress or comatose and unable to give any useful history.
In these cases, the clinician must rely upon the nature of the presentation and the presence of metabolic derangements and must always keep a high index of suspicion for toxic alcohol poisoning. Direct assays for the toxic alcohols are seldom available and gold standard test for the determination of serum toxic alcohol levels is gas chromatography.
Most hospitals do not have the ability to obtain this in a timely fashion and so we can not use it in the acute setting. Therefore, we must rely on clues to make the diagnosis, including osmol gap, anion gap, and acid-base status.
Pearls and pitfalls in the Emergency Department
Anion Gap:
- Anion gap is neither sensitive nor specific for diagnosing toxic alcohol poisoning.
- The values are dependent upon time of ingestion, which is often unknown.
- Soon after ingestion, the patient may manifest symptoms of toxic alcohol ingestion without an anion gap metabolic acidosis.
- The metabolic acidosis increases as the toxic alcohols are metabolized to organic acids creating an inverse relationship between the serum anion gap and osmol gap.
- The process of metabolism of toxic alcohols to organic acids can be slow with acidosis developing as late as 16 – 20 hours post ingestion.
Osmol Gap:
- Osmol gap is neither sensitive nor specific for diagnosing toxic alcohol poisoning.
- The range of “normal” for the osmol gap varies (usually 10 – 20 mOsm/L depending on the source).
- The differential diagnosis for elevated osmol gap is wide as any osmotically active substance present in the blood can lead to higher than normal serum osmolality (ketoacidosis, acute renal failure, chronic renal disease, lactic acidosis, mannitol, and shock).
- The absence of an osmol gap does not exclude toxic alcohol poisoning because blood-alcohol levels that are sufficient to cause clinical abnormalities may not markedly elevate the osmol gap.

Take home points:
- Toxic alcohol poisonings are rare, and their presentation is variable making diagnosis difficult. The best way to catch these cases is to keep them in your differential.
- Calculate an anion gap and osmolar gap, but remember depending on time of presentation from ingestion, these can be variable
- Fomepizole has a low side effect profile – if your clinical suspicion is high for toxic alcohol ingestion, consider giving it (remember ethanol can be used if fomepizole is not available).
- Isopropyl alcohol is the exception – treatment is typically supportive care.
- Call Poison Control! Toxicology is there to help!

